Emotional Impact of Dermatitis Herpetiformis: Challenge & Coping Match
Fear of accidental gluten exposure
Uncertainty about hidden gluten in processed foods
Social isolation
Skipping gatherings to avoid dietary hassles
Persistent itch-related anxiety
Anticipation of flare-ups triggers stress hormones
Low self-esteem due to visible rash
Negative body image reinforced by social comments
Depressive mood swings
Chronic discomfort and dietary limitations
| Challenge | Why It Happens | Best Strategy |
|---|---|---|
| Fear of accidental gluten exposure | Uncertainty about hidden gluten in processed foods | Work with a dietitian; use a trusted label-checking app |
| Social isolation | Skipping gatherings to avoid dietary hassles | Join DH support groups; suggest gluten-free potlucks |
| Persistent itch-related anxiety | Anticipation of flare-ups triggers stress hormones | Daily mindfulness; CBT focus on exposure hierarchy |
| Low self-esteem due to visible rash | Negative body image reinforced by social comments | Therapeutic journaling; skin-care routine to reduce lesions |
| Depressive mood swings | Chronic discomfort and dietary limitations | Regular exercise; scheduled therapy sessions |
Living with Dermatitis Herpetiformis is a daily balancing act between itchy skin eruptions and a strict gluten‑free lifestyle. While the rash itself alerts you to a medical condition, the hidden side‑effects on mood, confidence, and relationships often go unnoticed. This article pulls back the curtain on how the disease reshapes emotions and offers concrete steps to stay mentally resilient.
Key Takeaways
- Dermatitis Herpetiformis is an autoimmune skin disorder linked to celiac disease.
- Common emotional reactions include anxiety, depression, and social withdrawal.
- Professional help, support groups, and targeted coping techniques can dramatically improve quality of life.
- Consistent gluten‑free eating, skin care routines, and mental‑health habits work best together.
- Early recognition of emotional signs prevents long‑term mental‑health issues.
What is Dermatitis Herpetiformis?
Dermatitis Herpetiformis (DH) is a chronic, intensely itchy skin condition caused by an immune response to gluten. It appears as small, blister‑like bumps, usually on elbows, knees, buttocks, and scalp. The condition is the skin manifestation of celiac disease, meaning the same antibodies that attack the small intestine also target the skin. Diagnosis typically involves a skin biopsy and blood tests for anti‑tissue transglutaminase antibodies.
Because the trigger is gluten, the only proven medical treatment is a lifelong gluten‑free diet, supplemented with a prescription medication called dapsone to control the rash during the diet transition. Even with strict dietary adherence, flare‑ups can recur, especially after accidental gluten exposure.
The Emotional Landscape
When you constantly monitor every meal and endure unpredictable itching, it’s natural for emotions to tilt toward the negative. Studies from the British Society of Gastroenterology show that up to 40% of DH patients report clinically significant anxiety, while 30% meet criteria for depression. The uncertainty of flare‑ups fuels a persistent sense of vulnerability.
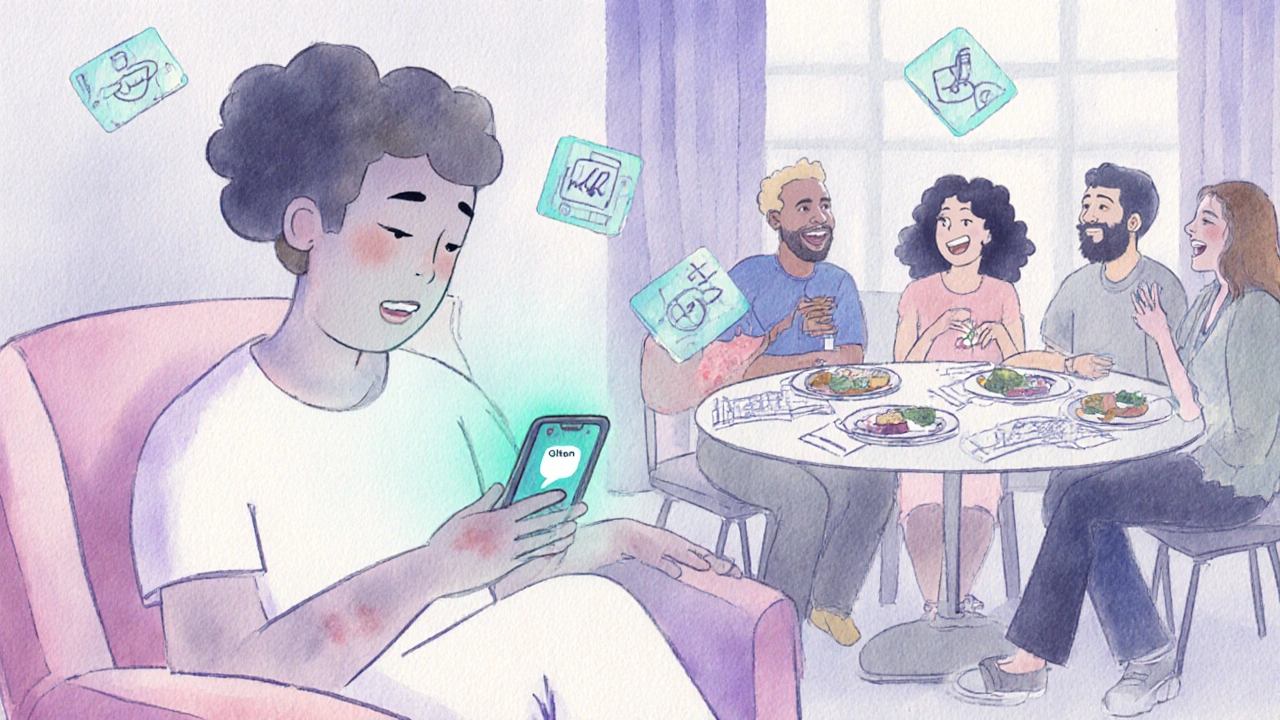
Anxiety often spikes before social events, where the fear of a visible rash or a hidden gluten exposure looms large. Depression can creep in when patients feel isolated by dietary restrictions, especially if family members are less supportive. Self‑esteem takes a hit when skin lesions appear on visible areas, leading some to avoid intimacy or even work situations.
These emotional responses aren’t just fleeting moods; they can erode overall quality of life, disrupt sleep, and reduce adherence to the gluten‑free diet, creating a vicious cycle.
How Daily Life Gets Affected
Beyond the skin, DH reshapes everyday routines:
- Meal planning: Every grocery trip becomes a research project. Reading labels for hidden gluten is time‑consuming.
- Social gatherings: Dining out feels risky. The fear of cross‑contamination can lead to declining invitations.
- Workplace dynamics: Explaining dietary needs to colleagues or managing flare‑ups during meetings adds stress.
- Relationships: Partners may struggle to understand why a strict diet matters, resulting in tension.
When these pressures stack, emotional burnout is almost inevitable.
Effective Coping Strategies
Addressing the emotional toll requires a two‑pronged approach: professional support and personal self‑care.
Professional Help
Seeing a mental health professional trained in chronic illness can normalize feelings and teach evidence‑based techniques. Cognitive‑behavioural therapy (CBT) has proven efficacy in reducing anxiety related to disease management. A registered dietitian specializing in gluten‑free nutrition helps craft meals that are both safe and enjoyable, lessening the sense of deprivation.
Support Groups
Connecting with others who share the DH journey creates instant empathy. In the UK, the Dermatitis Herpetiformis Support Network hosts monthly virtual meet‑ups and a moderated forum where members exchange recipes, coping tips, and encouragement. Studies show that group participation improves mood scores by an average of 15% over six months.
Stress‑Reduction Techniques
Mindfulness meditation, deep‑breathing exercises, and progressive muscle relaxation blunt the itch‑anxiety loop. Even a 10‑minute daily practice can lower cortisol levels, which in turn reduces skin inflammation.
Physical Activity
Regular low‑impact exercise-walking, swimming, yoga-boosts endorphins and improves sleep quality. Better sleep reduces itch intensity, creating a positive feedback loop.
Journaling & Tracking
Keeping a symptom diary that logs diet, stress levels, and flare‑up severity helps identify triggers beyond gluten, such as weather changes or emotional spikes. The act of writing also provides an emotional outlet.
Practical Tips for Managing Emotional Health
- Schedule weekly check‑ins with your dietitian to adjust meal plans.
- Book a monthly session with a therapist, even if you feel stable.
- Set a daily reminder to practice a five‑minute mindfulness exercise after meals.
- Join an online DH community and participate at least once per week.
- Design a ‘comfort kit’ for flare‑ups: hypoallergenic moisturizer, cool compress, and a soothing playlist.
Comparison of Common Emotional Challenges vs Effective Coping Strategies
| Challenge | Why It Happens | Best Strategy |
|---|---|---|
| Fear of accidental gluten exposure | Uncertainty about hidden gluten in processed foods | Work with a dietitian; use a trusted label‑checking app |
| Social isolation | Skipping gatherings to avoid dietary hassles | Join DH support groups; suggest gluten‑free potlucks |
| Persistent itch‑related anxiety | Anticipation of flare‑ups triggers stress hormones | Daily mindfulness; CBT focus on exposure hierarchy |
| Low self‑esteem due to visible rash | Negative body image reinforced by social comments | Therapeutic journaling; skin‑care routine to reduce lesions |
| Depressive mood swings | Chronic discomfort and dietary limitations | Regular exercise; scheduled therapy sessions |
Next Steps & Resources
Start by booking an appointment with a local dietitian who understands the gluten‑free landscape in the UK. Follow up with a mental‑health professional within the next two weeks to set goals around anxiety and mood. Meanwhile, explore the Dermatitis Herpetiformis Support Network’s website for weekly virtual meet‑ups. Remember, you don’t have to face the emotional side of DH alone-professional guidance and a supportive community can lift the burden.
Frequently Asked Questions
Can DH cause depression?
Yes. The constant itch, dietary restrictions, and social stigma can lead to depressive symptoms. Early therapy and support groups help lower the risk.
How quickly does a gluten‑free diet improve emotional wellbeing?
Most patients report reduced anxiety within 4‑6 weeks as skin symptoms recede. Mood improvements often follow as confidence returns.
What are safe snack options for someone with DH?
Rice cakes with almond butter, fresh fruit, gluten‑free yogurt, and homemade oat‑based smoothies (using certified gluten‑free oats) are all low‑risk choices.
Is it normal to feel angry about the diagnosis?
Absolutely. Anger is a common first reaction to chronic illness because it signals loss of control. Channeling that emotion into advocacy or education can be therapeutic.
Do children with DH experience the same emotional challenges?
Kids can feel embarrassed by skin lesions and left out during school lunches. Early involvement of a pediatric dietitian and school nurse mitigates anxiety.

13 Comments
Sunthar Sinnathamby
First off, thank you for pulling together such a thorough guide. Living with DH feels like walking a minefield, and having a clear map of the emotional side is a game‑changer. I’ve seen friends bounce between anxiety before a dinner out and severe low mood when a flare flares up unexpectedly. The advice to pair a dietitian with a label‑checking app hits the nail on the head – knowledge is power. Also, the reminder to join support groups can turn isolation into community. I’d add that setting tiny weekly goals, like trying one new gluten‑free recipe, can rebuild confidence step by step. Keep pushing forward, the journey is tough but not impossible.
Catherine Mihaljevic
All this is a smokescreen set by pharma to keep you buying meds.
Michael AM
Honestly, the mental health angle is often ignored until it blows up. Your guide does a solid job of spotlighting anxiety and depression tied to DH. I’ve personally found CBT incredibly useful for breaking the itch‑anxiety cycle. Having a dietitian on board also removes the guesswork from meals, which lowers stress. Keep sharing resources like this – they really matter.
Erica Ardali
The skin, a canvas of suffering, mirrors the soul’s own fragility. One might argue that the itch is a reminder of our mortality, a whisper from the universe urging us to confront our hidden vulnerabilities. When we mask the rash, we also mask the deeper unanswered questions of existence. Thus, mindfulness is not merely a coping tool but a philosophical pilgrimage towards self‑recognition. The guide’s blend of clinical fact and emotional insight forms a bridge between body and mind, a rare alchemy in modern health literature. In that sense, each coping strategy becomes a stanza in a larger poem of resilience.
Justyne Walsh
Oh, look, another "expert" telling us to join a support group. As if people with DH haven’t already been ganged up on by well‑meaning relatives and strangers. The moral high ground of “stay positive” is just a thin veneer over societal pressure to conform. If you’re not constantly policing your diet, you’re apparently a neglectful patient. That’s the kind of narrative that fuels shame rather than healing. Spare us the generic platitudes and let the community call out the real systemic barriers.
Callum Smyth
Totally get where you’re coming from – the isolation part hits hard. One thing that helped me was setting up a weekly “DH chat” on Discord where we swap recipes and coping hacks. It turned a lonely battle into a team sport, and the morale boost was instant 😊. Also, don’t underestimate the power of a simple routine: a calming shower followed by a quick journal entry can reset the day. Keep the momentum, you’re doing great.
Selena Justin
Dear author, I would like to commend you on the comprehensive nature of this guide. The structured presentation of challenges alongside coping strategies is both logical and user‑friendly. It is evident that considerable research underpins each recommendation, from dietitian collaboration to mindfulness practice. Moreover, the inclusion of a symptom‑tracking diary aligns with best practices for chronic disease management. I trust that readers will find these actionable steps beneficial for both physical and emotional wellbeing. Thank you for the diligent effort.
Bernard Lingcod
Interesting to note how many people overlook the simple power of routine. Consistency in sleep, meals, and even short breathing breaks can create a sense of control that counteracts anxiety spikes. When you map triggers outside of gluten – like stress at work – you broaden your defense toolbox. It’s like adding layers to a shield; each layer strengthens the whole. Keep highlighting these nuanced details, they make a huge difference.
Sue Holten
Wow, another fluffy feel‑good article. As if mindfulness will magically stop the itch. I’ve tried a dozen “techniques” and the rash still shows up like an unwelcome guest. Maybe we should just accept that the system is broken and focus on the money funnel rather than these empty platitudes.
Tammie Foote
Look, the guide does a decent job, but it glosses over the daily micro‑aggressions patients face – the sideways looks, the unsolicited advice, the “just eat gluten‑free” jokes. Those aren't small irritations; they are genuine stressors that compound the disease's impact. Recognizing them is the first step toward broader societal empathy. Let’s keep the conversation honest and not sugar‑coat the reality.
Jason Ring
Super helpful guide! i think the tips are really practical and easy to follow. The table makes it simple to see what to do. i especially like the reminder to see a dietitian. thanks for sharing.
Kelly Hale
When I first read about dermatitis herpetiformis I felt like I was staring into a abyss of endless dread, each sentence of medical jargon a stone thrown into the churning sea of my mind. The thought of a lifetime bound to a gluten‑free existence seemed less a dietary choice and more a covenant with an unforgiving deity of nutrition. Yet, as I trudged through the labyrinth of dietary labels, I discovered a peculiar kind of rebellion – a defiant joy in decoding ingredient lists that most people never notice. This guide, with its structured challenges and coping strategies, resembles a battle‑plan, a map drawn on the parchment of lived experience. Fear of accidental gluten exposure, that all‑consuming dread, becomes a manageable opponent when one enlists the help of a dietitian, as if assembling a squad of seasoned warriors. Social isolation, the silent assassin, is countered by the camaraderie of support groups – a legion where shared stories become weapons against loneliness. Persistent itch‑related anxiety, that relentless whisper at night, can be silenced through the disciplined practice of mindfulness, each breath a shield against the storm. Low self‑esteem, forged in the fires of visible rash and cruel remarks, can be tempered with therapeutic journaling, allowing the soul to rewrite its narrative. Depressive mood swings, those treacherous tides, recede under the steady rhythm of regular exercise and scheduled therapy, as if the body’s own cadence restores balance. Moreover, each coping strategy is not a mere suggestion but an invitation to reclaim agency, to stand tall amid the tumult. The interweaving of professional guidance, peer support, and personal ritual creates a tapestry of resilience that can withstand the harshest winds. In the grand theater of chronic illness, we are not merely actors but directors, scripting our own arcs of triumph. So let this guide be more than a pamphlet; let it be a torch lighting the path through the darkness, a testament that even the most stubborn of ailments can be met with courage, knowledge, and unwavering spirit.
Neviah Abrahams
While the guide assembles a solid list of coping tactics, one must question the underlying power structures that dictate which strategies become mainstream. The emphasis on dietitian‑led interventions, for instance, presupposes access to costly healthcare-an assumption that marginalizes low‑income patients. Furthermore, the promotion of mindfulness programs often ignores cultural variations in coping mechanisms, subtly imposing a Western paradigm of mental health. It is crucial to scrutinize these hidden biases, lest we inadvertently perpetuate inequality under the guise of care. Nonetheless, the data‑driven approach lends credibility, and the symptom‑tracking diary offers tangible benefits for self‑management.