Every year, thousands of people end up in emergency rooms because of unexpected reactions between their prescription drugs and the supplements they take. It’s not always obvious - you might be taking milk thistle for your liver, turmeric for inflammation, or a multivitamin you think is harmless. But when those mix with blood thinners, antidepressants, or chemotherapy drugs, the results can be dangerous. The good news? You don’t have to guess. There are specialized drug interaction databases built specifically to catch these conflicts - if you know how to use them.
Why checking supplement interactions isn’t optional
More than half of U.S. adults take dietary supplements. Among people over 55, nearly half are on at least one prescription medication and one supplement at the same time. That’s not just common - it’s a ticking time bomb if you don’t check for interactions. A 2015 study in JAMA Internal Medicine found that supplement-drug interactions cause about 23,000 emergency room visits each year in the U.S. alone. Many of these are preventable. The problem isn’t the supplements themselves - it’s the lack of awareness. Patients rarely mention them to their doctors, and many providers don’t ask. But when you’re on warfarin, apixaban, or statins, even something as simple as ginkgo biloba or St. John’s wort can change how your body processes your meds - sometimes with life-threatening results.What makes a good supplement interaction database?
Not all drug interaction tools are created equal. Most general databases like DrugBank or DDInter focus on drug-drug interactions and treat supplements as an afterthought. They might list a few common ones like garlic or vitamin E, but they miss the real problem: proprietary blends. Take a product labeled “Liver Support Complex.” It might contain milk thistle, dandelion, artichoke, and turmeric - all in different doses. Most databases won’t recognize the product name. But if you know the ingredients, you can check each one. That’s where NatMed (formerly Natural Medicines) stands out. NatMed maps over 1,900 dietary supplements to their exact ingredients. It doesn’t just say “ginkgo.” It tells you if the product contains 120 mg of ginkgo flavone glycosides and 24 mg of terpene lactones - and whether that combination interacts with your anticoagulant. In clinical validation studies, NatMed achieved 94.3% inter-rater reliability among pharmacists - meaning different experts using the same tool almost always agree on the risk level. No other database comes close.Step 1: Get a full list of everything you’re taking
Start with the patient - or yourself. Don’t rely on memory. Ask for every pill, capsule, powder, tincture, or tea. Include:- Prescription drugs
- Over-the-counter meds (like ibuprofen or antacids)
- Dietary supplements (vitamins, minerals, herbs)
- Probiotics and fish oil
- Energy drinks or weight-loss formulas
- Topical creams or patches with active ingredients
Step 2: Identify the exact ingredients
This is where most people fail. You can’t search “Nature’s Way Omega-3” in a database and get accurate results. Databases don’t recognize brand names. They recognize ingredients. Look at the Supplement Facts label. Find the active ingredients. If it says “proprietary blend,” you’re in trouble. That means the manufacturer won’t tell you how much of each herb or nutrient is in there. In those cases, you have two options:- Ask the patient where they bought it - sometimes the brand website lists full ingredients
- Use a third-party verification tool like NSF International or USP Verified - they test products for label accuracy
Step 3: Enter the ingredients into a trusted database
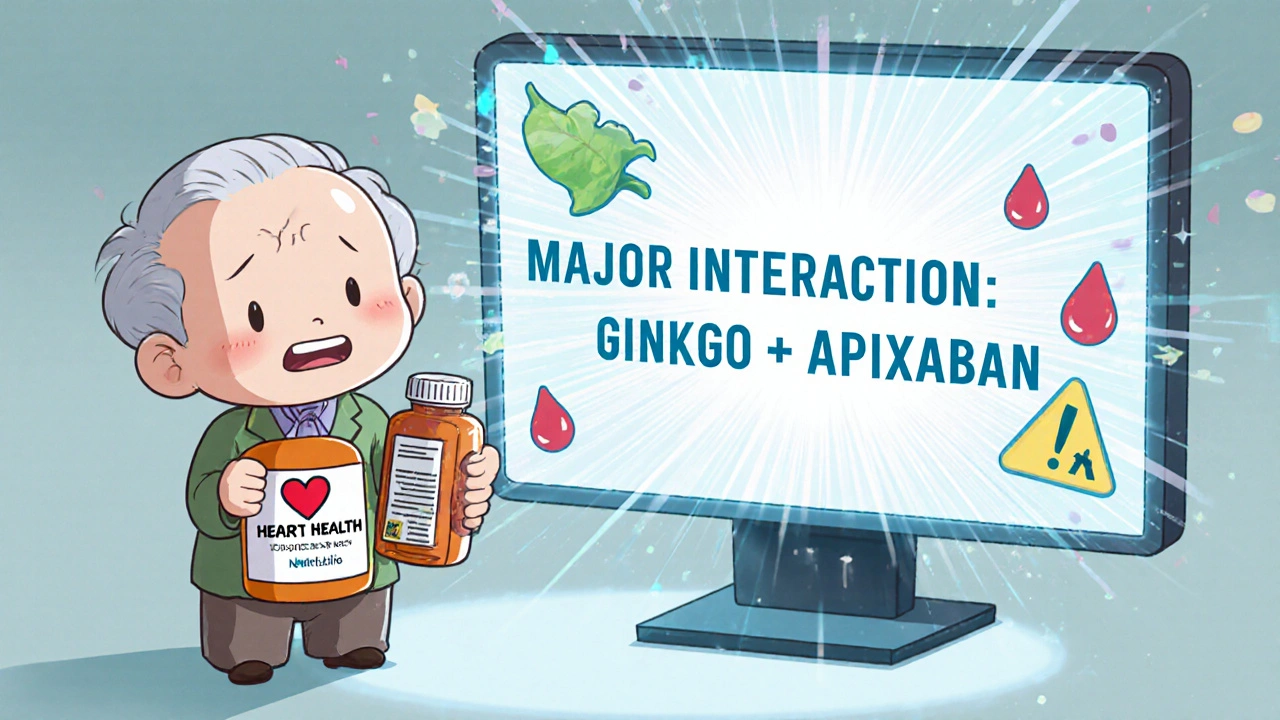
Now, open NatMed (available at natmed.therapeuticresearch.com). Log in. Go to the “Supplement Interaction Checker.” Type in the ingredient - not the brand. For example, type “ginkgo biloba,” not “Ginkgo Biloba Extract by Nature’s Bounty.” The system will auto-suggest the correct entry. Click on it. Then, add your medication - say, “apixaban.” The system will immediately show you:- Severity level: Major
- Mechanism: Ginkgo inhibits platelet aggregation and may increase bleeding risk when combined with anticoagulants
- Management: Avoid concurrent use. If unavoidable, monitor for bruising, nosebleeds, or blood in stool
Step 4: Cross-check with all medications
Don’t stop at one drug. Run every medication through the same process. A patient on metformin, lisinopril, and simvastatin might be fine with one supplement - but together, those drugs can create a perfect storm. For example:- St. John’s wort + simvastatin = reduced statin levels → higher cholesterol risk
- Calcium + levothyroxine = poor thyroid absorption → need to space doses by 4 hours
- Green tea extract + beta-blockers = increased heart rate and blood pressure
Step 5: Interpret the severity levels
Not all interactions are equal. NatMed uses a clear four-tier system:- Contraindicated: Do not use together. High risk of death or serious harm.
- Major: Avoid if possible. Requires close monitoring or dose adjustment.
- Moderate: Use with caution. May cause side effects but usually manageable.
- Minor: Low risk. No action needed unless patient is sensitive.
Step 6: Document and communicate
Once you’ve checked everything, write it down. Include:- Supplement name and exact ingredient
- Medication it interacts with
- Severity level
- Recommended action
- Alternative supplement (if applicable)

What to do when the database doesn’t know
Sometimes, you’ll hit a blank. That happens with newer supplements - like CBD, ashwagandha extracts, or adaptogenic blends. As of Q2 2024, only 37% of CBD-drug interactions were documented in commercial databases. In those cases:- Check PubMed or the NIH’s LiverTox database for case reports
- Look for studies on CYP450 enzyme inhibition - that’s how 62% of serious interactions happen
- Use pharmacokinetic principles: If the supplement affects liver enzymes (CYP3A4, CYP2D6), it likely affects your meds
8 Comments
Julia Strothers
Let me guess - NatMed is just another FDA shill tool. They don't want you to know that 90% of these 'interactions' are manufactured by Big Pharma to kill off natural remedies. Ginkgo biloba? It's been used for 4,000 years. The real danger is that your statin is poisoning your liver while the FDA approves it. They're scared of supplements because they don't make money off them. You think they'd let a free, effective alternative exist? Wake up. This whole 'database' is a control mechanism. They want you dependent on pills - not plants. I've seen people die from prescriptions. I've never seen someone die from turmeric. The system is rigged.
Erika Sta. Maria
ok so u said natmed is gld standard but did u kno that it costs 2000$ a yr?? like wtf?? how is that accesible to normal people?? also i used it once and it said 'no interaction' for ashwagandha + prozac but my cousin had a seizure after mixing them so... maybe the '94.3% reliability' is just marketing fluff? also why do all these databases ignore ayurvedic herbs? they're not in the system but they're in my grandma's medicine cabinet. capitalism > science. 🤷♀️
Nikhil Purohit
Really appreciate this breakdown - I’ve been using NatMed at work for the past year and it’s been a game-changer. I used to just Google things and guess, but now I’ve got concrete data. One guy on warfarin was taking a ‘heart tonic’ with ginseng - turned out it was a major interaction. We switched him to hawthorn berry, which has zero known interactions. He’s doing great now. The key is just being thorough. Don’t skip Step 1 - people forget their gummy vitamins or that herbal tea they drink at night. Those are the ones that get you.
Debanjan Banerjee
Julia and Erika - your comments are dangerously misinformed. NatMed isn’t a corporate tool; it’s a clinically validated, peer-reviewed database used by hospitals, pharmacists, and poison control centers. The cost? Yes, it’s expensive - but it’s funded by institutions, not individuals. If you can’t access it, ask your pharmacist - many libraries and clinics offer free access. As for ayurvedic herbs, they’re being added incrementally as evidence emerges. The FDA doesn’t regulate supplements - that’s why we need tools like NatMed to fill the gap. Ignoring evidence because it’s inconvenient doesn’t make you wise - it makes you reckless. This isn’t about capitalism. It’s about preventing death.
Steve Harris
Great guide - very clear and practical. I’ve been a nurse for 18 years and I still get surprised by how often patients hide their supplement use. One lady told me she only took 'a little fish oil' - turned out she was taking 6,000 mg a day with her blood thinner. We caught it because we asked specifically. I always use the 10-item checklist now. It’s not about being paranoid - it’s about being thorough. And yeah, NatMed is the best. I wish every ER had it. The AI name recognition update? Huge. Saved me 3 hours last week.
Michael Marrale
Wait… so you’re telling me that if I take CBD oil for my anxiety, and I’m on Zoloft, and I eat grapefruit, and I drink green tea, and I take magnesium… I could just randomly drop dead without knowing? And the government doesn’t even require labels to say that? And NatMed only has 37% of CBD interactions logged? That’s not a database - that’s a death lottery. And you’re telling me to trust it? What if the database is hacked? What if it’s owned by the same people who make antidepressants? What if they’re hiding the real interactions? I’ve seen things. I know things. You think this is about health? It’s about control. They want you docile. They want you dependent. Don’t believe the hype.
David vaughan
I just wanted to say… thank you. I’ve been on 5 meds for years, and I never thought to check supplements. I took melatonin with my blood pressure pill for a year. No idea it could raise my BP. Found out because I read this. Now I use NatMed every time I buy something new. Even if it’s just a 'natural energy boost' from the gas station. I screenshot every result. I print it. I bring it to my doctor. I know it sounds obsessive… but I’d rather be safe than sorry. I’m alive because I checked. Seriously - do it. It’s not paranoia. It’s self-respect.
David Cusack
How quaint. A step-by-step guide to navigating the pharmaceutical-industrial complex’s curated illusion of safety. NatMed? A glorified proprietary database masquerading as science. One must ask: who funds it? Who controls the evidence thresholds? The 94.3% inter-rater reliability is statistically meaningless if the raters are all trained within the same ideological framework. And the FDA’s blockchain pilot? A performative gesture to appease the digitally gullible. Real knowledge lies in primary literature - not in commercial interfaces designed to extract subscription fees. One might as well consult a horoscope for drug interactions. At least it’s honest about its lack of empirical basis.