When a brand-name drug loses patent protection, patients and pharmacists often expect a flood of cheap generics. But sometimes, the first version to hit the shelf isn’t a traditional generic at all-it’s an authorized generic. These aren’t knockoffs. They’re the exact same pills, capsules, or injections as the brand-name drug, just sold under a different label. And in 2025, the number of new authorized generics has dropped sharply-leaving patients and providers to wonder what’s really available and why.
What Exactly Is an Authorized Generic?
An authorized generic is made by the same company that produces the brand-name drug. It uses the same active ingredients, same inactive ingredients, same manufacturing process, and same quality controls. The only difference? The packaging and label. Instead of the flashy brand name, it might say something like ‘Pregabalin 75 mg’ with no logo. It’s still the exact same product you’d get from the brand, just cheaper.
The FDA defines it clearly: it’s a drug approved under a New Drug Application (NDA) that’s then sold under a different label. Unlike traditional generics-which require an Abbreviated New Drug Application (ANDA) and can have different fillers or coatings-authorized generics don’t need to prove bioequivalence. They’re already proven because they’re made by the brand company itself.
This matters for patients on drugs with narrow therapeutic windows-like seizure meds, blood thinners, or thyroid hormones. Even tiny changes in inactive ingredients can cause side effects or reduced effectiveness. Many patients report no issues switching from brand to traditional generic, but others notice subtle differences. With an authorized generic, there’s no guesswork.
Why Are There So Few New Authorized Generics in 2025?
In 2022, the FDA listed 37 new authorized generics. In 2025? Just 12. That’s a 68% drop in just three years.
The reason isn’t lack of demand. It’s regulation. The Federal Trade Commission (FTC) has been cracking down on what it calls ‘pay-for-delay’ tactics. In the past, brand companies would sometimes launch their own authorized generic right before a traditional generic entered the market. This strategy would scare off competitors by flooding the market with a low-priced version-while still keeping profits through their own label. The FTC called it anti-competitive. And they’ve been winning in court.
The 2023 $1.2 billion settlement with Teva over Copaxone was a turning point. Since then, big pharma has backed off. Launching an authorized generic now carries legal risk. Instead, companies are shifting to biosimilars-especially for biologics like Stelara or Humira. In 2025 alone, five interchangeable biosimilars to Stelara were approved. But biosimilars aren’t authorized generics. They’re different products, with different manufacturing processes and slightly different structures.
What Authorized Generics Are Actually Available Now?
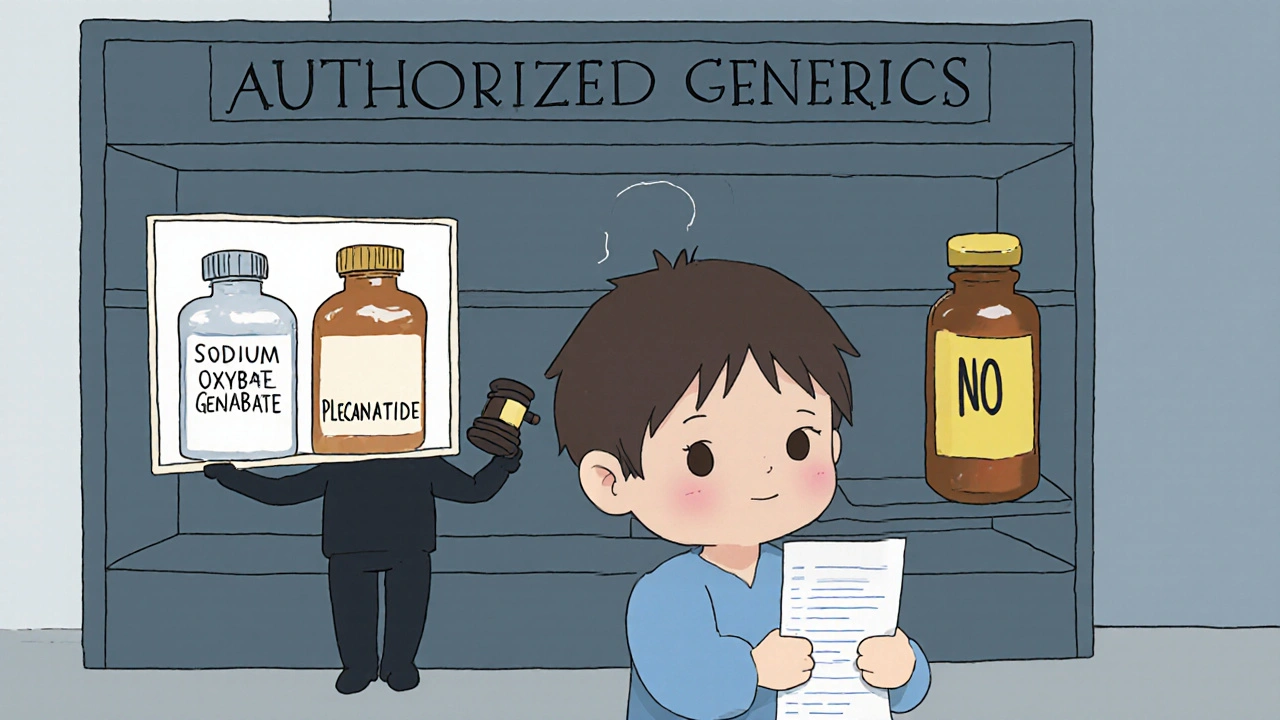
As of October 2025, the FDA’s official list includes 1,247 authorized generics. Only two new ones were added this year:
- Sodium oxybate (Xyrem) - marketed by Jazz Pharmaceuticals under a different label
- Plecanatide (Trulance) - distributed by Ironwood Pharmaceuticals
These aren’t flashy new drugs. They’re older, established treatments for rare conditions. Sodium oxybate treats narcolepsy and cataplexy. Plecanatide helps with chronic constipation. Neither is a blockbuster drug, so the financial incentive to block competition was low.
For popular medications like Lyrica (pregabalin), Jardiance (empagliflozin), or Sertraline, authorized generics exist-but they’ve been around for years. For example, Pfizer’s authorized generic of sertraline has been on the market since 2019. It’s still available, still identical to Zoloft, and still cheaper. But no new ones have entered since.
Are Authorized Generics Actually Cheaper?
Here’s the catch: they’re cheaper than the brand, but not always cheaper than traditional generics.
A 2025 Health Affairs study found authorized generics typically cost 10-15% less than the brand. Traditional generics? Often 80% less. That’s a huge gap. So why do they exist at all?
Because pharmacies and insurers don’t always push them. Insurance companies negotiate rebates with generic manufacturers. The bigger the rebate, the more the PBM (pharmacy benefit manager) wants to steer patients toward that version-even if it’s not identical. One Reddit user reported their insurer, Blue Cross BCBS, dropped coverage for the authorized generic of Jardiance, forcing patients back to the brand or a traditional generic-even though the authorized version was chemically identical.
On Drugs.com, users of the authorized generic of Lyrica gave it a 4.2/5 rating. 68% said it worked exactly like the brand. But 78% said it was only $5 cheaper at their pharmacy. That’s not enough to motivate a switch.
Why Pharmacists Struggle to Identify Them
Here’s a problem no one talks about: most pharmacists can’t tell an authorized generic from a traditional one just by looking at the bottle.
A 2025 survey of 2,345 pharmacists found 63% couldn’t reliably distinguish them without checking the FDA’s Orange Book. That’s a big deal. Pharmacists are supposed to counsel patients when switching medications. But if they don’t know they’re switching from a brand to an authorized generic-because the label looks like a generic-they might give unnecessary warnings. Or worse, they might not warn at all when switching to a traditional generic with different fillers.
Some states are starting to respond. The Community College of Philadelphia now includes a 3-hour module on identifying authorized generics in its pharmacy technician program. Other schools are likely to follow.

Who Benefits the Most From Authorized Generics?
Patients on drugs where even small changes can cause problems. Think epilepsy, Parkinson’s, or psychiatric medications. For these, formulation consistency isn’t a luxury-it’s a safety net.
Dr. Aaron Kesselheim of Harvard Medical School calls authorized generics an ‘underutilized patient safety tool.’ He’s right. In a world where 80% of prescriptions are filled with generics, the fact that we still have a version that’s 100% identical to the brand should be a big deal. But it’s not marketed that way. No ads. No patient brochures. No push from insurers.
And that’s the tragedy. The system has the tool. But it’s not using it.
The Future: Will Authorized Generics Disappear?
Most experts say yes-if current trends continue. Evaluate Pharma predicts authorized generics will make up less than 5% of new generic entries by 2027. The FTC is still active. The pending RELIEF Act (H.R. 4086) would force authorized generics to match the price of traditional generics. That removes the financial incentive for brand companies to make them at all.
Meanwhile, biosimilars are taking over. They’re complex, expensive to develop, and require years of testing. But they’re the new battleground for drug companies trying to extend market control without violating antitrust laws.
For patients, the takeaway is simple: if you’re on a brand-name drug that just went generic, ask your pharmacist: Is there an authorized generic available? It might not be cheaper, but it might be safer. And if your insurance won’t cover it, ask why. Sometimes, the only thing standing between you and the exact same medication you’ve always taken is a rebate deal between a pharmacy benefit manager and a generic manufacturer.
Authorized generics aren’t the future of generics. But for now, they’re the most reliable version of the past.
What’s the difference between an authorized generic and a regular generic?
An authorized generic is made by the same company that produces the brand-name drug, using the exact same ingredients and manufacturing process. A regular generic is made by a different company and may use different inactive ingredients (fillers, dyes, coatings), even though the active ingredient is the same. Authorized generics are chemically identical to the brand; regular generics only need to prove they work the same way in the body.
Are authorized generics always cheaper than the brand?
Yes, but not always by much. Authorized generics typically cost 10-15% less than the brand-name version. Traditional generics, on the other hand, often cost 80% less. The price advantage of authorized generics is small, which is why insurers sometimes prefer traditional generics-even if they’re not identical.
How do I know if my prescription is an authorized generic?
Check the label. Authorized generics usually have no brand name on the bottle-just the generic drug name. But the best way is to ask your pharmacist or check the FDA’s Authorized Generics list online. Many pharmacists can’t tell just by looking, so don’t assume. If your pill looks different from your last refill, ask if it’s an authorized generic.
Why aren’t authorized generics more common today?
Because the FTC has cracked down on brand companies using them to block competition. In the past, companies would launch an authorized generic right before a cheaper generic entered the market to scare off competitors. That practice is now legally risky. As a result, few companies are launching new authorized generics-only 12 in 2025, down from 37 in 2022.
Can I ask my doctor to prescribe an authorized generic?
Yes, but your doctor may not know which one it is. You’ll need to tell them the name of the brand drug you’re taking and ask if there’s an authorized generic available. Then, ask your pharmacist to fill it. Some insurance plans won’t cover it unless you’ve tried the cheaper traditional generic first. So you might need to appeal.
Are authorized generics safe for long-term use?
Yes. Because they’re identical to the brand-name drug, they’re just as safe and effective for long-term use. Many patients who switched from brand to traditional generic report side effects like dizziness, nausea, or mood changes-symptoms that disappeared when they switched back to the authorized generic. For drugs with narrow therapeutic windows, this consistency matters.
If you’re managing a chronic condition and your medication just went generic, don’t assume all generics are the same. Ask for the authorized version. It might not be the cheapest-but it’s the most predictable.

11 Comments
Kevin Wagner
Let me tell you something-authorized generics are the silent heroes of pharma. I’ve been on Lyrica for years, and when my pharmacy switched me to the authorized version, I didn’t notice a difference. Zero. Not a headache, not a dip in mood, nothing. Meanwhile, the regular generic? I felt like I was walking through molasses for two weeks. Same active ingredient, sure-but the fillers? Total crap. Why aren’t more people talking about this?
gent wood
It’s frustrating, isn’t it? The system is designed to save money, but it often sacrifices consistency-and for patients with epilepsy or bipolar disorder, that’s not just inconvenient, it’s dangerous. I work in a GP practice in London, and we’ve seen a spike in patients returning with destabilized symptoms after switching to non-authorized generics. The FDA’s list is a start, but pharmacists need better training, and insurers need to stop prioritizing rebates over safety.
Dilip Patel
USA always overcomplicate everything. In India, we get generic medicine for 10 rupees and it works fine. Why you need same pill with different label? You people think too much. If medicine works, why care who made it? Pharma companies cheat you with brand names and now this authorized thing? Just take the cheap one and stop complaining. Also, biosimilars are for rich people. Real medicine is simple.
Jane Johnson
It’s ironic that a system designed to reduce costs has created a more complex, opaque landscape. The lack of transparency in labeling, combined with insurer-driven formularies, undermines patient autonomy. Furthermore, the regulatory environment has incentivized strategic withdrawal rather than innovation. This is not progress; it’s regulatory arbitrage disguised as competition.
Sean Hwang
My mom’s on sertraline. Switched from Zoloft to the authorized generic a few years back. No issues. She didn’t even know it was different until I showed her the bottle. Pharmacist didn’t say anything either. I think most people wouldn’t notice unless they’re super sensitive. The real problem? Insurance won’t cover it unless you try the $3 generic first. So even if you want the safe one, you gotta jump through hoops. Sad.
Barry Sanders
Let’s be real: authorized generics are a corporate loophole. Brand companies use them to delay real competition. The fact that they’re ‘identical’ doesn’t make them ethical-it makes them strategic. And now we’re pretending they’re some kind of patient safety tool? Please. It’s profit with a placebo label.
Chris Ashley
Bro I just asked my pharmacist last week if my Jardiance was the authorized one and he looked at me like I spoke Klingon. Then he said ‘it’s generic, that’s all that matters.’ I told him the brand and the authorized one are the same pill, just different label-he didn’t even know what I was talking about. How are we supposed to advocate for ourselves if the people filling our scripts don’t know the difference?
kshitij pandey
From India, I want to say: this is beautiful. You people care about medicine quality even when it costs more. In our country, we just take what’s available and are thankful. But your system, even with its flaws, shows that patients matter. Keep pushing for transparency. Maybe one day, we’ll learn from you. And yes, authorized generics? They’re like the quiet uncle who always shows up-no fanfare, but always there when you need him.
Brittany C
Per the FDA Orange Book, authorized generics are classified under NDA-listed products with no ANDA submission. Their bioequivalence is pre-established by virtue of identical manufacturing. This distinguishes them from ANDA-based generics, which may demonstrate bioequivalence via dissolution profiles and pharmacokinetic studies. The clinical implications are significant for narrow-therapeutic-index agents, particularly in neurology and endocrinology. However, reimbursement structures remain misaligned with therapeutic fidelity.
Anjan Patel
It’s disgusting how big pharma plays games with our lives. They let us suffer with bad generics, then act like they’re saints when they release an authorized version. And now the FTC’s cracking down? Good. But why wait until people are harmed? This isn’t about competition-it’s about control. They don’t care if you’re stable. They care if you’re paying. And we’re all just pawns in their profit game.
Scarlett Walker
My doctor didn’t even know what an authorized generic was. I had to show her the FDA list. She was like, ‘Oh, so that’s what that is!’ We got it covered now-insurance still tried to push the $5 generic, but I appealed. Took two weeks. Worth it. I feel like a different person. No brain fog. No nausea. Just… normal. If you’re on meds that affect your mind or body, don’t settle. Ask. Fight. It matters.