Most people assume that if a drug is available as a generic, it’s just as good-and cheaper. And for the vast majority of medications, that’s true. But there are times when your doctor insists on the brand-name version, even if a generic exists. You might wonder why. Is it just about profit? Or is there something more serious going on?
When Generics Aren’t Enough
It’s not about brand loyalty. It’s about biology. Some drugs work so precisely that even tiny differences in how they’re absorbed can cause big problems. These are called narrow therapeutic index (NTI) drugs. For these, the difference between a safe dose and a dangerous one is razor-thin.Think of it like tuning a piano. If a string is just a little off, the whole note sounds wrong. For medications like levothyroxine (Synthroid), warfarin (Coumadin), or levetiracetam (Keppra), even a 10% change in blood levels can mean the difference between control and crisis. A patient on Synthroid might feel fine one month, then develop fatigue, weight gain, or depression after switching to a generic made by a different company. That’s not just bad luck-it’s a real risk.
The FDA says generics must be within 80-125% of the brand’s absorption rate. That sounds tight, but for NTI drugs, that 45% window is too wide. The American Thyroid Association and the American Academy of Neurology both recommend sticking with the same brand for these drugs. Why? Because switching between generics-even ones approved by the FDA-can cause unpredictable changes in how your body responds.
Why Doctors Still Use Brand Names
Doctors don’t prescribe brand-name drugs lightly. It’s expensive-for patients and the system. But sometimes, the cost of switching is higher than the cost of staying put.One reason is patient history. If you’ve been on Synthroid for years and your thyroid levels are stable, your doctor isn’t going to risk changing it. Same with epilepsy patients on Keppra. A 2019 study tracked 1,200 people who switched from brand to generic levetiracetam. Nearly 13% had breakthrough seizures. Only 4% did when they stayed on the brand. That’s not a small difference. That’s life-changing.
Another reason is inactive ingredients. Generics use the same active drug, but they can have different fillers, dyes, or coatings. For some people, those extras cause reactions. One patient on Reddit described how switching from brand to generic ciprofloxacin gave them severe stomach cramps and nausea. The generic had a different binder. The brand didn’t. After switching back, the symptoms vanished.
Then there’s the delivery system. Some drugs come in special devices-like Advair’s Diskus inhaler or Humira’s pre-filled pen. Even if the active ingredient is the same, the way it’s delivered matters. A generic version of the drug might not work with the same device. So if your inhaler doesn’t release the right dose, the medication fails. That’s not a generic issue-it’s a design issue.

How Much Do Brand-Name Drugs Really Cost?
The price gap is staggering. In 2022, the average brand-name prescription cost $471.67. The generic? $13.76. That’s over 97% cheaper. For statins like atorvastatin, switching to generic saved people an average of $1,200 a year. That’s a car payment. A month’s rent. A year’s worth of insulin for some.But here’s the catch: insurance doesn’t always make it easy. If your doctor writes “do not substitute” or “brand medically necessary,” your insurer might require prior authorization. That means paperwork, waiting 72 hours, and sometimes getting denied. For antiepileptics, approval rates are high-nearly 90%. For proton pump inhibitors? Only 45%.
And even if approved, you might still pay more. Some plans charge higher copays for brand-name drugs unless you’ve tried and failed with the generic first. That’s called step therapy. It’s meant to save money-but it can delay treatment. And if you’re already stable on a brand, forcing you to switch can backfire.
What the Research Really Says
Let’s be clear: for most drugs, generics are just as good. A 2020 JAMA study looked at 47 trials with over 112,000 patients. They compared brand and generic versions of blood pressure meds, cholesterol drugs, and diabetes pills. No difference in outcomes. Not a single one.But that’s not the whole story. A 2018 study of over a million doctor’s notes found that physicians prescribed brand names 15-20% of the time-even when it wasn’t medically needed. Why? Because they’re used to saying the brand name. “We say ‘Lipitor’ instead of ‘atorvastatin’ because it’s easier,” said Dr. David Ouyang from Stanford. “And once you say it, you’re more likely to prescribe it.”
Drug companies know this. They spend millions training reps to get doctors to say brand names. They give out free samples. They put logos on everything. It’s marketing dressed up as medicine.
Dr. Caleb Alexander from Johns Hopkins put it bluntly: “Only about 3% of brand-name prescriptions have real clinical justification.” That means 17% of the time, people are paying hundreds of dollars more for no medical reason.

What You Can Do
If your doctor prescribes a brand-name drug, ask: “Is this medically necessary?” Don’t be afraid to push back. You have the right to know why.Ask these questions:
- Is this drug on the FDA’s list of narrow therapeutic index drugs?
- Have I had problems with generics before?
- Is there a generic that’s been proven to work for me?
- Can we try the generic and monitor my response?
If your doctor says yes to any of those, they’re likely right. But if they say, “It’s just better,” or “I’ve always prescribed it this way,” dig deeper.
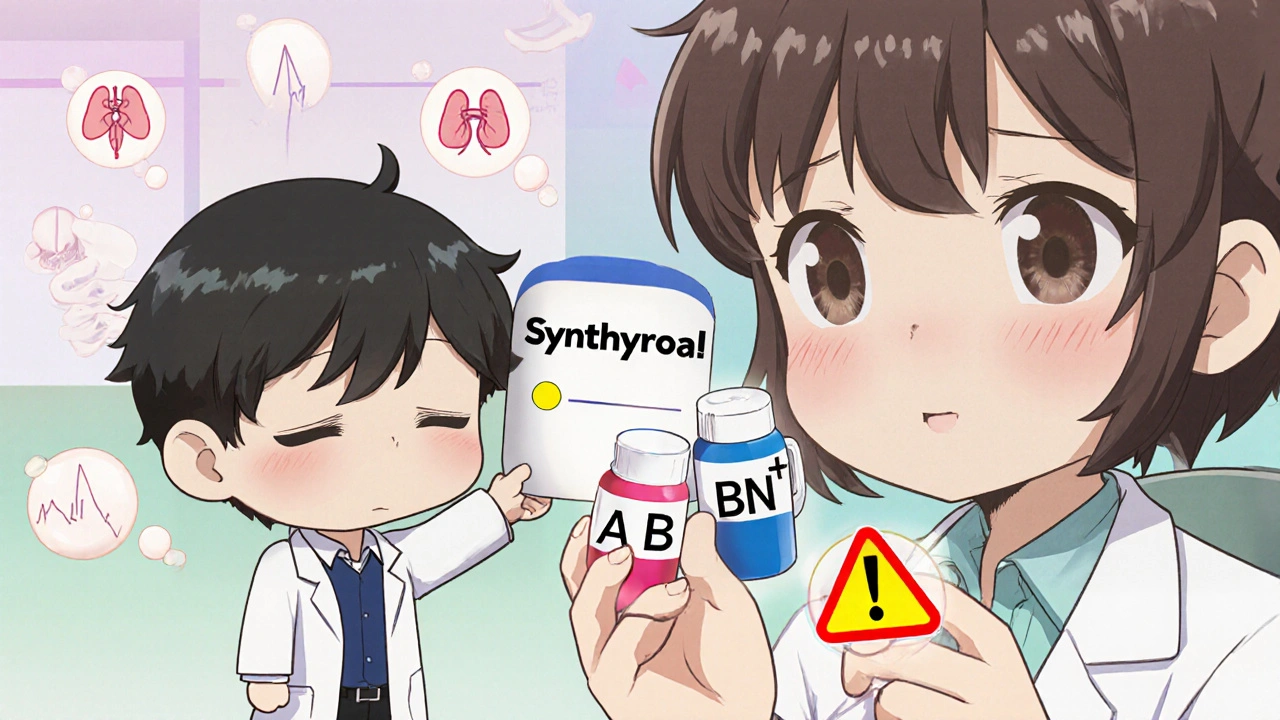
Check the FDA’s Orange Book. It lists which generics are rated as therapeutically equivalent to brand-name drugs. You can ask your pharmacist to show you the rating. If it says “AB,” it’s interchangeable. If it’s “BN” or unlisted, that’s a red flag.
Also, keep a record. If you switch to a generic and feel worse-fatigue, dizziness, mood changes, seizures-write it down. Note the date, the drug name, and the manufacturer. Bring it to your next appointment. That’s real data. And it matters.
What’s Changing
The system is slowly waking up. In 2023, the FDA started requiring generic manufacturers to match the shape and color of brand-name pills. Why? Because patients confuse look-alike drugs. One study found 34% of medication errors came from mixing up pills because they looked different.There’s also a rise in “authorized generics”-the same drug, made by the brand company, sold under a generic label. These avoid the variability between different generic makers. They’re not cheaper than other generics, but they’re more consistent. Some insurers are starting to cover them as a middle ground.
And prescriber education is improving. Electronic health records now flag when a drug has a narrow therapeutic index. But a 2022 study showed those alerts only reduced inappropriate prescribing by 18.7%. That’s progress-but not enough.
For now, the best defense is knowledge. Know your drugs. Know your body. And don’t assume that just because a generic exists, it’s always the right choice.
Can pharmacists substitute a generic if my doctor writes ‘brand only’?
No. If your doctor writes “do not substitute,” “dispense as written,” or “brand medically necessary,” the pharmacist is legally required to fill the brand-name version. This rule applies in all U.S. states except Texas, which has additional requirements for certain drug classes. Pharmacists cannot override a prescriber’s explicit instruction.
Are all generics the same?
No. While all generics must contain the same active ingredient as the brand, they can differ in fillers, dyes, binders, and coatings. These inactive ingredients don’t affect how the drug works-but they can affect how your body tolerates it. Some people react to certain fillers, leading to stomach upset, rashes, or other side effects. That’s why switching between different generic manufacturers can sometimes cause problems.
What are narrow therapeutic index (NTI) drugs?
NTI drugs are medications where even small changes in blood levels can lead to serious side effects or treatment failure. Examples include levothyroxine (for thyroid), warfarin (for blood thinning), phenytoin and levetiracetam (for seizures), and lithium (for bipolar disorder). For these, switching between brands or generics can be risky, so doctors often recommend sticking with one version.
Why do some doctors always prescribe brand-name drugs?
Some doctors prescribe brand-name drugs out of habit, familiarity, or because they’ve seen patients react poorly to generics in the past. Others are influenced by pharmaceutical marketing. Drug reps often promote brand names and provide samples, making them more top-of-mind. But research shows that for most drugs, this isn’t medically necessary. Only about 3% of brand prescriptions have strong clinical justification beyond patient or provider preference.
Can I ask my doctor to switch me to a generic?
Yes, absolutely. If your medication isn’t on the narrow therapeutic index list and you’re not experiencing side effects, asking to switch to a generic is a smart, cost-saving move. Many common drugs-like metformin, lisinopril, and atorvastatin-work just as well in generic form. If your doctor refuses without a clear reason, ask for evidence. You have the right to understand why a more expensive option is being chosen.
What should I do if I have side effects after switching to a generic?
If you notice new or worsening symptoms after switching to a generic-like fatigue, mood changes, dizziness, or seizures-document them. Write down the date, the drug name, the manufacturer (check the pill bottle), and how you’re feeling. Bring this to your doctor. It’s possible the generic isn’t working for you, and you may need to go back to the brand or try a different generic. Never ignore new side effects. Your body is telling you something.
15 Comments
Kezia Katherine Lewis
NTI drugs are a minefield. The FDA’s 80-125% bioequivalence window is a statistical abstraction that ignores individual pharmacokinetic variance. For levothyroxine, even a 5% fluctuation in serum T4 can trigger subclinical hypothyroidism-fatigue, weight gain, cognitive fog. The American Thyroid Association’s stance isn’t arbitrary; it’s evidence-based. Switching generics isn’t a cost-saving measure-it’s a clinical gamble with your homeostasis.
And don’t get me started on inactive ingredients. One patient I consulted had chronic GI distress from a generic levetiracetam because of the colloidal silicon dioxide binder. Switch back to Synthroid or Keppra? Symptoms vanished. The pill looks the same. The active ingredient is identical. But biology doesn’t care about your formulary.
This isn’t about brand loyalty. It’s about pharmacodynamics, inter-individual variability, and the fact that the body isn’t a test tube.
Insurers pushing step therapy for NTI drugs are engaging in predatory cost-shifting. The downstream costs-ER visits, hospitalizations, lost productivity-far exceed the savings.
Know your drug’s therapeutic index. Ask for the Orange Book rating. If it’s AB, fine. If it’s BN or unlisted? Push back. Your physiology deserves precision, not economies of scale.
Henrik Stacke
Oh my goodness, this is absolutely spot-on. I’ve been on warfarin for eight years now. Switched to a generic once-just once-because my pharmacy ‘recommended’ it. Three days later, my INR spiked to 5.8. I ended up in A&E with a nosebleed that wouldn’t stop. The nurse asked if I’d changed meds. I said no. She checked my bottle. ‘Ah,’ she said, ‘you’ve got the generic from Company X.’
I haven’t touched a generic since. My GP now writes ‘Do Not Substitute’ in bold, underlined, and circled. I don’t care if it costs £120 a month. I’d rather pay for peace of mind than risk a stroke because someone thought ‘close enough’ was good enough.
And yes, the marketing? Oh, absolutely. My cardiologist once said, ‘I prescribe Coumadin because I’ve seen what happens when it goes wrong.’ Not because he’s paid by Bristol-Myers. Because he’s seen patients die.
Thank you for writing this. It’s not just about pills. It’s about trust in medicine.
Manjistha Roy
As someone who manages thyroid disease and has seen multiple generics fail, I can confirm: consistency matters. I switched from Synthroid to a generic, and my TSH went from 2.1 to 8.7 in six weeks. No change in diet, no change in sleep, no change in stress. Just the pill. I went back to Synthroid. TSH returned to baseline in four weeks.
Also, the inactive ingredients-some generics use lactose. I’m lactose intolerant. I didn’t realize that until I started bloating and getting diarrhea every time I took the generic. The brand? No issue. The generic? I had to read the label. No one told me.
Pharmacists don’t always know the difference between AB-rated and BN-rated generics. And patients? We assume all pills with the same name are the same. They’re not.
Always check the manufacturer. Always document symptoms. Always ask for the Orange Book rating. And if your doctor says, ‘It’s fine,’ ask them to show you the study that proves it for YOU.
Knowledge is power. And in this case, it’s survival.
Jennifer Skolney
I had a seizure after switching to generic levetiracetam. Not a little twitch. A full-on tonic-clonic. I woke up in the ER with my mom crying and a nurse asking if I’d changed meds. I said no. She checked the bottle. ‘Oh. You’re on the generic now.’
I cried for an hour. Not because I was scared. Because I felt stupid. I trusted the system. I trusted ‘generic = same.’
Now I keep a binder. Every pill. Every manufacturer. Every date I switched. Every symptom. I bring it to every appointment. My neurologist says I’m the most organized patient he’s ever had. I say I’m the only one who survived the system’s laziness.
Don’t let anyone tell you it’s ‘just a pill.’ It’s your brain. Your body. Your life.
And yes, I still use emojis when I’m angry. 😤
JD Mette
Interesting read. I’ve been on atorvastatin for ten years. Switched to generic in 2018. No issues. My LDL is rock solid. I’ve never felt different. So I get why some people need brand. But for most? It’s fine.
I think the problem is we treat all meds like they’re the same. They’re not. Some are sensitive. Some aren’t. The key is knowing which is which.
Also, the cost difference is insane. I saved over $800 a year. That’s a vacation. Or groceries for a month.
So maybe the answer isn’t ‘always brand’ or ‘always generic.’ Maybe it’s ‘know your drug, know your body, and talk to your doctor.’
Simple. But hard to do.
Olanrewaju Jeph
It is a matter of pharmacological precision, not corporate greed. The narrow therapeutic index of drugs such as levothyroxine, warfarin, and phenytoin necessitates consistent bioavailability. Variability in dissolution rates among generic manufacturers, even within FDA guidelines, can result in subtherapeutic or toxic concentrations.
The 80–125% bioequivalence window is statistically acceptable for most drugs, but for NTI agents, it is clinically unacceptable. The American Academy of Neurology and the American Thyroid Association have issued clear guidelines on this matter, and these are grounded in peer-reviewed clinical data.
Additionally, excipients-such as lactose, magnesium stearate, or hypromellose-can trigger adverse reactions in individuals with sensitivities. These are not inert substances; they are pharmacologically active in the context of individual physiology.
Therefore, when a physician prescribes a brand-name drug with a ‘do not substitute’ directive, it is not a reflection of bias, but of clinical responsibility.
Patients must be empowered to request the Orange Book classification and to document any changes in symptoms following a switch. This is not paranoia. It is evidence-based self-advocacy.
Dalton Adams
Let’s be real. Most doctors prescribe brand names because they’re lazy. They don’t want to look up the Orange Book. They don’t want to explain to a patient why their $400 pill is ‘necessary.’ They just say ‘Synthroid’ because that’s what they learned in med school in 1998.
And don’t even get me started on pharma reps. They show up with free samples, branded pens, and $20 Starbucks cards. You think your doctor doesn’t notice that? Of course he does. He’s human.
Meanwhile, I’ve been on generic metformin for 12 years. No issues. Generic lisinopril? Perfect. Generic omeprazole? I’ve taken five different brands. Zero problems.
So stop pretending every generic is a death sentence. Only 3% of brand prescriptions are medically necessary. That means 97% of the time, you’re paying for a logo.
And yes, I’ve seen people die from switching generics. But I’ve also seen people go bankrupt because they were too scared to save $1,200 a year.
Balance. Not fear. Not greed. Balance.
Also, 🤷♂️
Kane Ren
This is such an important topic. I used to think generics were just as good-until my sister had a seizure after switching to a generic version of her epilepsy med. She was fine for years on Keppra. Then one day, out of nowhere-convulsions. Turned out the generic had a different binder. She went back to brand. No more seizures.
It’s not about being anti-generic. It’s about being pro-safety.
And honestly? If you’re saving $100 a month but risking your health, is it really worth it?
Knowledge is power. Ask questions. Track your symptoms. Don’t let anyone make you feel silly for caring.
You’re not being difficult. You’re being smart.
And hey-you’re worth the extra cost. 💪
Adrian Rios
Let me tell you about my cousin. She’s been on levothyroxine since she was 19. 27 now. Switched to a generic because her insurance ‘forced’ it. Within two weeks, she was exhausted. Couldn’t get out of bed. Weight gain. Hair falling out. She thought she was depressed. Went to therapy. Got antidepressants. Nothing helped.
Then she found this article. Read the part about NTI drugs. Called her endocrinologist. Said, ‘I think the generic is killing me.’
Switched back. Three weeks later, she was back to normal. No meds. No therapy. Just the right pill.
Doctors don’t always know this stuff. Pharmacies don’t warn you. Insurance doesn’t care.
So if you’re on a thyroid med, an anticonvulsant, or warfarin-don’t assume. Don’t trust. Ask. Document. Fight.
This isn’t about money. It’s about your life.
And if someone tells you it’s ‘just a pill’? Tell them to go read the JAMA study. Then tell them to come back when their INR is 6.0 and they’re bleeding out.
Stay vigilant. Stay loud. Stay alive.
Brandy Walley
Generic = same. My ass.
shreyas yashas
I’m from India. We don’t have brand-name drugs here. Everything’s generic. But we have this weird thing-we call the brand name even when we take the generic. Like, ‘I take Synthroid’-but it’s actually the local version made by Sun Pharma.
Turns out, some of these generics are actually made in the same factories as the US brand. Just sold under a different label.
So maybe the problem isn’t the generic. It’s the lack of transparency. We don’t know who made it. Where. How.
Maybe the solution isn’t ‘stick to brand.’ Maybe it’s ‘demand traceability.’
Also, my aunt took a generic for hypertension. She got dizzy. Switched back to the brand. Fine. But the brand here costs 10x more. So she stopped taking it. Now she has high BP.
It’s not black and white. It’s a mess.
But we still need to talk about it.
Suresh Ramaiyan
There’s a deeper question here: Why do we treat medicine like a commodity? We buy groceries in bulk. We compare prices for cars. But when it comes to our bodies, we’re told to trust the system.
But the system isn’t designed for healing. It’s designed for efficiency.
NTI drugs are the exception that exposes the rule: medicine is not engineering. It’s biology. And biology doesn’t care about your budget.
Maybe the real problem isn’t the generics. It’s that we’ve outsourced our health to a machine that doesn’t understand nuance.
So yes-ask questions. Demand records. Track symptoms.
But also-ask why we’re being forced to choose between health and affordability.
That’s the real crisis.
Not the pill. The system.
Katy Bell
I didn’t know any of this until my mom had a stroke. She was on warfarin. Switched to generic because her Medicare plan said so. Didn’t tell her the risks. Didn’t warn her.
She didn’t even know she’d switched. Thought it was the same pill.
Now she’s on brand. Forever. And I’m mad.
Not at the doctors. Not at the pharmacists.
At the system.
Why didn’t anyone tell us? Why is this not common knowledge?
And why do we have to be the ones to fight for our own safety?
I’m not angry. I’m just… tired.
But I’m still here. And I’m not letting anyone else get blindsided like she did.
Ragini Sharma
so like… i switched my generic cipro to a different brand n got super dizzy? then i switched back n it was fine? so… yeah. generics r not all the same. but also why does my insurance make me try 3 diff ones before letting me have the one that works? 😭
Kezia Katherine Lewis
And that’s exactly why step therapy is dangerous. It’s not ‘try before you approve.’ It’s ‘hurt before you help.’
My endocrinologist told me once: ‘If you’re stable on Synthroid, you’re not a candidate for a switch. You’re a candidate for protection.’
Insurance doesn’t see patients. They see claims. And they optimize for the lowest cost per claim, not the best outcome per life.
So when you’re denied prior authorization for your brand-name drug? That’s not bureaucracy. That’s negligence dressed in paperwork.
Document everything. Submit appeals. If they deny it, go to your state’s insurance commissioner. They have to respond.
And if your doctor won’t fight for you? Find one who will.
Because your life isn’t a spreadsheet.