Levothyroxine Dose Adjustment Calculator
This calculator helps you understand how proton pump inhibitors (PPIs) may affect your levothyroxine absorption based on clinical evidence. Studies show that when you take both medications, your body may absorb less thyroid hormone, which can lead to elevated TSH levels. This may require a dose adjustment of 12.5-25 mcg per day for many patients.
Recommended Adjustment
Based on clinical evidence:
- 15-20% of patients on both medications need dose increases
- Typical adjustment range: 12.5-25 mcg per day
- Adjustments are often needed within 6-8 weeks of starting PPIs
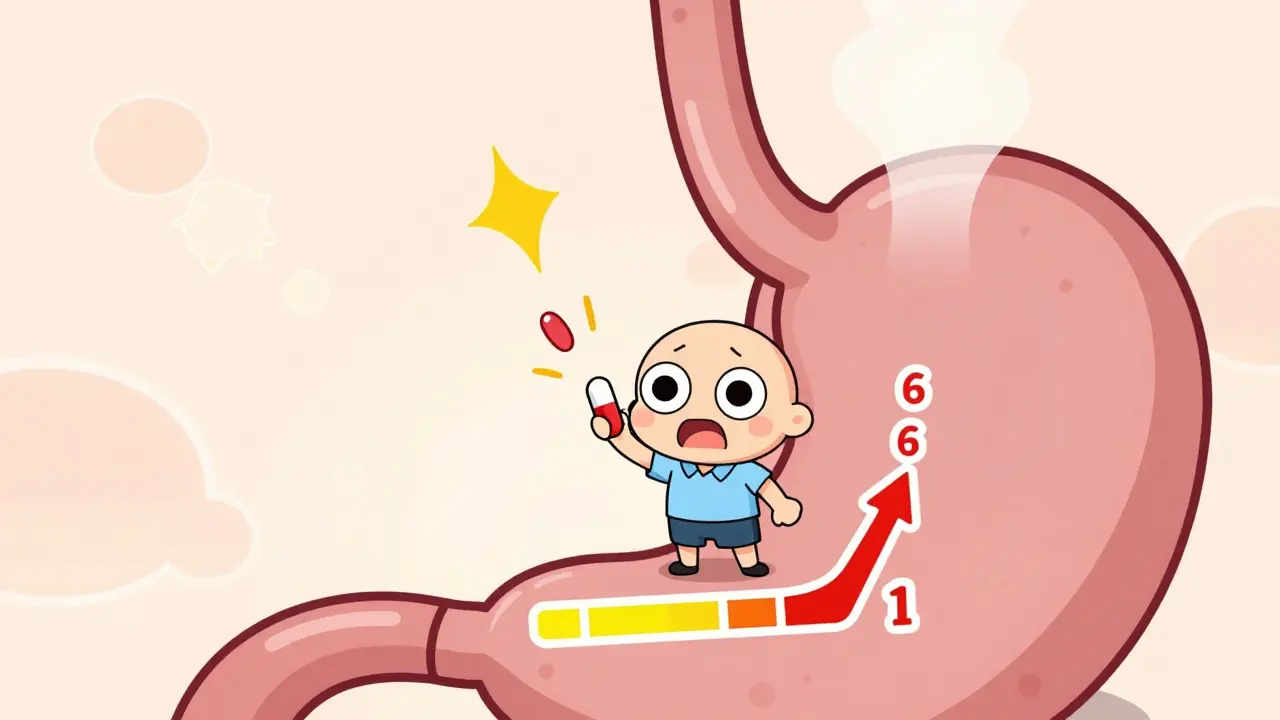
If you're taking levothyroxine for hypothyroidism and also use a proton pump inhibitor (PPI) like omeprazole or pantoprazole for heartburn, you might be unknowingly reducing how well your thyroid medication works. This isn’t just a theoretical concern-it’s a real, documented interaction that affects millions of people. Studies show that when these two drugs are taken together, your body absorbs less levothyroxine, which can push your TSH levels up and leave you feeling tired, gaining weight, or struggling with brain fog-even if you’re taking your pill every day exactly as prescribed.
Why Levothyroxine Needs Acid to Work
Levothyroxine isn’t like most pills. It doesn’t just dissolve and get absorbed anywhere in your gut. It needs a very acidic environment-think pH 1 to 2-to break down properly and enter your bloodstream. That’s why it’s usually taken on an empty stomach, first thing in the morning, with a full glass of water. The stomach’s natural acid helps dissolve the tablet so your body can absorb it in the small intestine.
Proton pump inhibitors (PPIs) shut down the acid-producing pumps in your stomach lining. Drugs like omeprazole (Prilosec), esomeprazole (Nexium), and pantoprazole (Protonix) are powerful. They don’t just reduce acid for a few hours-they can keep your stomach near-neutral (pH 4-6) for up to 72 hours after a single dose. That’s long enough to interfere with levothyroxine absorption, even if you take them hours apart.
What Happens When You Take Them Together
A 2021 systematic review in the Journal of General Internal Medicine looked at seven clinical studies involving over 1,200 patients. Every single one found that people taking both levothyroxine and a PPI had higher TSH levels than when they took levothyroxine alone. Higher TSH means your thyroid isn’t getting enough hormone signal-your body is basically screaming for more thyroid medication.
One 2023 study followed patients on 40mg of pantoprazole daily for six weeks. Even though they took levothyroxine in the morning and pantoprazole at night, their TSH still jumped. That’s because PPIs don’t just act when you take them-they change your stomach’s chemistry for days. Timing doesn’t fix it. Separating doses by four or even six hours won’t help if your stomach isn’t acidic enough when the pill passes through.
Research from the Mayo Clinic Proceedings found that about 15-20% of patients on both medications need their levothyroxine dose increased. The average bump? 12.5 to 25 micrograms per day. That’s a full half-tablet or more for many people. If your doctor doesn’t know about this interaction, they might think your hypothyroidism is getting worse-when really, your medication just isn’t being absorbed.

Who’s Most at Risk?
It’s not just anyone on PPIs. If you’ve been taking them for more than three months, you’re in the high-risk group. Short-term use (under four weeks) usually doesn’t cause problems. But long-term users-those taking PPIs for GERD, ulcers, or even chronic bloating-are the ones who see the biggest drops in levothyroxine absorption.
According to IQVIA data, around 18% of the 15 million Americans on chronic levothyroxine also take a PPI. That’s nearly 2.7 million people. And based on Reddit’s r/Hashimotos community, 68% of patients who reported long-term PPI use said they had to increase their levothyroxine dose. Common symptoms? Fatigue (72%), unexplained weight gain (58%), and cold intolerance. These aren’t just "feeling off"-they’re signs your thyroid hormone levels are too low.
What Can You Do?
You don’t have to stop your PPI if you need it. But you do need to manage the interaction. Here are your options, ranked by evidence and practicality.
- Test your TSH before and after starting a PPI. The American Association of Clinical Endocrinologists recommends a baseline TSH test before starting a PPI, then another at 6-8 weeks. If your TSH is up, your dose likely needs adjustment. Many patients stabilize within 12 weeks after a dose change.
- Consider switching to famotidine (Pepcid). Unlike PPIs, H2 blockers like famotidine don’t shut down acid production for days. A 2018 study in Pharmacotherapy showed no significant TSH changes when famotidine was taken with levothyroxine. It’s less powerful than PPIs, but if you don’t need maximum acid suppression, it’s a safer alternative.
- Switch to liquid levothyroxine. Tirosint-SOL is a liquid formulation that doesn’t need stomach acid to dissolve. A 2019 study in the Journal of Clinical Endocrinology & Metabolism confirmed it’s absorbed just as well whether taken with or without acid. The catch? It costs $350 a month compared to $15-$25 for generic tablets. Insurance often doesn’t cover it unless you’ve tried and failed with tablets.
- Don’t rely on timing. Taking your PPI at night and levothyroxine in the morning won’t fix this. The acid suppression lasts too long. Even studies that tested morning vs. evening PPI dosing found no difference in TSH levels.

What’s Coming Next?
The FDA is working on new labeling rules for thyroid medications to clearly warn about PPI interactions. That’s a big step toward making doctors and patients aware. Meanwhile, researchers are testing new formulations of levothyroxine-like enteric-coated pills-that bypass the stomach entirely and release the hormone in the intestine, where acid doesn’t matter. Phase 3 trials are underway, and if they succeed, this problem could become a thing of the past.
There’s also a looming market shift. Tirosint-SOL’s patent expires in 2025. Generic manufacturers are already working on similar liquid or capsule-based versions. If they succeed, access could improve dramatically. But as the Journal of Pharmaceutical Sciences pointed out in 2022, formulating a stable, bioavailable liquid levothyroxine isn’t easy. It’s not just about dumping the powder into water-it’s about chemistry that keeps the hormone intact and absorbable.
What to Do Right Now
If you’re on both medications:
- Check your last TSH result. If it’s been over 3 months, schedule a blood test.
- Ask your doctor if your PPI is still necessary. Could you reduce the dose? Try it every other day? Or switch to famotidine?
- If your TSH is high and you’re on a PPI, don’t assume your hypothyroidism is worsening. Ask if the interaction could be the cause.
- If you’re struggling with fatigue or weight gain despite taking your medication, mention your PPI use. It might be the missing piece.
This isn’t about avoiding PPIs. It’s about being smart about how you use them. Millions of people need acid suppression. Millions more need thyroid hormone. The problem isn’t the drugs-it’s how we’ve been taught to take them together without checking the impact. With a little testing and a few adjustments, you can get both your heartburn and your energy back.
Can I take levothyroxine and a PPI at the same time?
No, taking them together reduces how well your body absorbs levothyroxine. Even if you space them by several hours, PPIs suppress stomach acid for up to 72 hours, making timing ineffective. The best approach is to test your TSH levels and adjust your levothyroxine dose if needed, or consider switching to an alternative like famotidine or liquid levothyroxine.
Does every PPI affect levothyroxine the same way?
Yes. All proton pump inhibitors-omeprazole, esomeprazole, pantoprazole, lansoprazole, and rabeprazole-work the same way by blocking acid production. Studies have shown consistent TSH increases with all of them. The strength of the effect may vary slightly by dose, but the mechanism and outcome are the same across the class.
How long does it take for TSH to rise after starting a PPI?
TSH levels typically begin to rise within 2-4 weeks of starting a PPI, with the most significant changes seen by 6-8 weeks. That’s why guidelines recommend checking TSH at the 6-8 week mark after beginning PPI therapy. Waiting longer risks prolonged under-treatment of hypothyroidism.
Is liquid levothyroxine better than tablets if I’m on a PPI?
Yes, if you’re on long-term PPI therapy, liquid levothyroxine like Tirosint-SOL is more reliable because it doesn’t require stomach acid for absorption. Clinical studies confirm it delivers consistent hormone levels regardless of gastric pH. The downside is cost-it’s 15-20 times more expensive than generic tablets. Insurance coverage may require prior authorization or failure of tablet therapy first.
Can I stop my PPI to fix my thyroid levels?
Only if your doctor agrees it’s safe. Many people take PPIs for serious conditions like Barrett’s esophagus or recurrent ulcers. Stopping them suddenly can cause rebound acid hypersecretion and worsen symptoms. The goal isn’t to stop the PPI-it’s to adjust your thyroid treatment to account for it. Always work with your provider before making changes.
15 Comments
Ajay Brahmandam
This is one of those posts that makes you realize how much we take our meds for granted. I’ve been on levothyroxine for 8 years and started omeprazole last year for acid reflux. My TSH went from 2.1 to 7.8 in 3 months. My endo didn’t even blink until I brought this up. Now I’m on famotidine and back to normal. If you’re tired and gaining weight despite taking your pill, check this first.
jenny guachamboza
THE GOVERNMENT IS HIDING THIS. PPIs are just the beginning. They’re also poisoning your gut biome to make you dependent on thyroid meds so Big Pharma can sell you more 💊💀 #FreeThyroid #PPICoverup
Aliyu Sani
Man, this hits different. In Nigeria, most folks just swallow pills without knowing what they do. I’ve seen people on PPIs for years because they think heartburn is normal. But thyroid? That’s a silent killer. The body’s got its own chemistry, and we’re just hacking it with chemicals. We need more education, not just prescriptions.
Gabriella da Silva Mendes
Wow, so now we’re supposed to trust some random blog post over our doctor? In America, we’ve got board-certified endocrinologists who know what they’re doing. Meanwhile, you’re reading Reddit and thinking you’re a pharmacist now. And liquid levothyroxine? At $350? That’s a scam. Just take your pills like everyone else and stop overthinking. 🇺🇸
Kiranjit Kaur
Thank you for this! I’ve been feeling like a zombie for months and thought it was just stress. I switched from omeprazole to Pepcid last week and already feel lighter. My energy’s coming back. You’re not alone - and this isn’t normal fatigue. 🙌💛
Sam Black
There’s something poetic about how our bodies demand balance - acid for absorption, silence for clarity, space for healing. We treat pills like magic bullets, but biology doesn’t work in isolation. The stomach isn’t just a chute; it’s a gatekeeper. And when we silence it too long, the whole system stumbles. Maybe the real fix isn’t more drugs, but more listening.
Cara Hritz
Wait - you said pantoprazole? That’s not even a PPI lol. It’s an H2 blocker. I know this because I read it on WebMD once. Also, your TSH numbers are wrong. Normal is 0.4-4.0, not 2.1-7.8. You’re just scared of meds. 💅
Jamison Kissh
It’s fascinating how we’ve turned medicine into a scheduling problem. If only we could time our pills like coffee, right? But the body doesn’t care about your 7am alarm or your 10pm dinner. It cares about pH, surface area, and molecular solubility. We’re trying to outsmart evolution with alarms and spreadsheets. Maybe the real solution is simpler: fewer PPIs, more food, less anxiety.
Tony Du bled
I’m from Texas. We don’t do fancy liquid meds here. We take pills, drink water, and get on with life. But I’ve got a cousin on levothyroxine and PPIs - same story. TSH up, fatigue down. He switched to Pepcid and now he’s hiking again. No drama. Just common sense. If your doctor doesn’t know this, find a new one.
Kathryn Weymouth
Thank you for the meticulous detail. The 2021 systematic review in the Journal of General Internal Medicine is a critical reference, and the 2023 pantoprazole study is particularly compelling. I’ve shared this with my endocrinology team - we’re now implementing pre-PPI TSH screening protocols for all new patients on levothyroxine. Precision matters.
Nader Bsyouni
You think this is a medical issue? Nah. It’s a capitalist trap. Why would they let you fix your thyroid naturally when they can sell you a $350 bottle of liquid? They want you dependent. They want you confused. They want you paying for pills you don’t need. Wake up. The stomach doesn’t need acid. The body is self-healing. Just eat turmeric and stop believing in science.
Julie Chavassieux
I’ve been on both for 11 years. My TSH is 12. I’m crying. My dog doesn’t recognize me. My husband left. I can’t sleep. I tried everything. I even moved to Arizona. Nothing helped. Then I read this. I switched to Pepcid. And now… I’m alive again. Thank you. I’m not okay. But I’m trying.
Herman Rousseau
Big win for patient advocacy here. If you’re on a PPI and thyroid meds, DO NOT PANIC. But DO check your TSH. And if your doctor brushes you off, bring this post. Print it. Highlight it. Bring a friend. This isn’t just science - it’s your energy, your mood, your life. You deserve to feel like yourself again. 💪
Vikrant Sura
Typical. Another post pretending to be helpful while ignoring the real issue: people take meds because they’re lazy. Eat less junk. Stop stressing. Your stomach acid isn’t broken. You’re just weak. Also, liquid levothyroxine? That’s for rich people who think their problems are special.
Candy Cotton
While the information presented is technically accurate, it is presented in a manner inconsistent with the rigorous standards of clinical practice guidelines issued by the American Thyroid Association. The reliance on anecdotal Reddit data and non-peer-reviewed institutional reports undermines the credibility of the conclusions drawn. Patients must be advised to adhere strictly to physician-directed regimens, not algorithmic social media content.