Sirolimus Wound Healing Risk Calculator
Patient Risk Factors
Risk Assessment
When a patient gets a kidney transplant, the goal isn’t just to survive the surgery-it’s to thrive long-term. But one drug that helps protect the new organ, sirolimus, can also slow down the body’s ability to heal wounds. This creates a real dilemma for surgeons and transplant teams: how do you balance the need for immunosuppression with the risk of open incisions that won’t close properly?
How Sirolimus Slows Down Healing
Sirolimus, also known as rapamycin, works by blocking a protein called mTOR. This stops immune cells from attacking the transplanted organ, which is exactly what doctors want. But mTOR doesn’t just control the immune system-it’s also critical for wound healing. When you block it, you’re not just calming the immune response. You’re also slowing down skin repair, blood vessel growth, and collagen production. Studies in rats show that when sirolimus is given at therapeutic doses (2.0 to 5.0 mg/kg/day), wound breaking strength drops by up to 40%. That’s not a small effect. The drug reduces vascular endothelial growth factor (VEGF) by half or more. VEGF is the signal that tells blood vessels to grow into the wound. No VEGF? No new blood supply. No new blood supply? The wound can’t get oxygen or nutrients to rebuild tissue. Fibroblasts-cells that make collagen-also stop multiplying. And without collagen, the wound stays weak. What’s worse, sirolimus doesn’t just stay in the blood. It concentrates in wound fluid at two to five times the level found in the bloodstream. That means the wound is getting a direct, high-dose hit, even if the blood levels look fine.When Do Complications Happen?
The biggest risks show up in the first week after surgery. That’s when the body is trying to seal the incision, form new tissue, and fight off early infections. Sirolimus interferes with every step. Clinical reports from the 2000s showed high rates of wound dehiscence (incisions reopening), lymphoceles (fluid pockets), and infections in patients started on sirolimus right after transplant. One 2008 Mayo Clinic study looked at 26 transplant patients on sirolimus who had skin surgeries. Nineteen percent got infections. Seven point seven percent had their wounds split open. That’s higher than the control group, but the numbers were small, and the differences weren’t statistically significant. Still, those numbers scared a lot of doctors. Many centers started delaying sirolimus for at least 7 to 14 days after surgery. But here’s the twist: newer data suggests those early fears may have been overblown. The same 2008 study found no statistically significant increase in complications. And in 2022, researchers pointed out that many of the worst cases came from patients who were already at high risk-obese, diabetic, smokers, or malnourished. The drug wasn’t the only problem. It was the combination.Who’s at Highest Risk?
Not every transplant patient on sirolimus will have a bad outcome. Risk depends heavily on individual factors.- BMI over 30: Obesity increases the odds of wound problems by 2 to 3 times. Fat tissue has poor blood flow and more inflammation, making healing harder.
- Diabetes: High blood sugar damages small blood vessels and weakens immune defense in wounds.
- Smoking: Nicotine cuts off oxygen to tissues. Quitting 4 weeks before surgery can reduce complications by up to 50%.
- Protein malnutrition: Wound healing needs protein. Low albumin levels are a red flag.
- Age over 65: Healing slows naturally with age.

Timing Matters: When to Start Sirolimus
There’s no one-size-fits-all answer. But here’s what works in practice today:- For high-risk patients (obese, diabetic, smoker, poor nutrition): Delay sirolimus until day 10-14 post-op. Let the wound stabilize first.
- For low-risk patients (young, healthy, non-smoker, normal BMI): Some centers start sirolimus as early as day 5-7, especially if the surgery was low-risk (like a kidney transplant with a clean closure).
- For major abdominal surgeries: Wait at least 10 days. The risk of internal leaks or lymphoceles is too high earlier.
- For skin or minor procedures: Sirolimus may be safe even during early recovery. The Mayo Clinic study found no major issues in patients on sirolimus who had dermatologic surgeries.
Dosing and Monitoring
It’s not just when you start sirolimus-it’s how much you give. Higher blood levels mean more suppression of healing. Research now shows that keeping sirolimus trough levels below 4-6 ng/mL during the first 30 days after transplant reduces wound complications without increasing rejection risk. Many centers now check levels weekly in the early post-op period and adjust doses based on healing, not just rejection markers. Also, sirolimus doesn’t work alone. It’s often combined with steroids, mycophenolate, or even antithymocyte globulin (ATG). All of those drugs can also slow healing. The problem isn’t always sirolimus-it’s the cocktail. A patient on triple immunosuppression has a much higher risk than someone on sirolimus alone.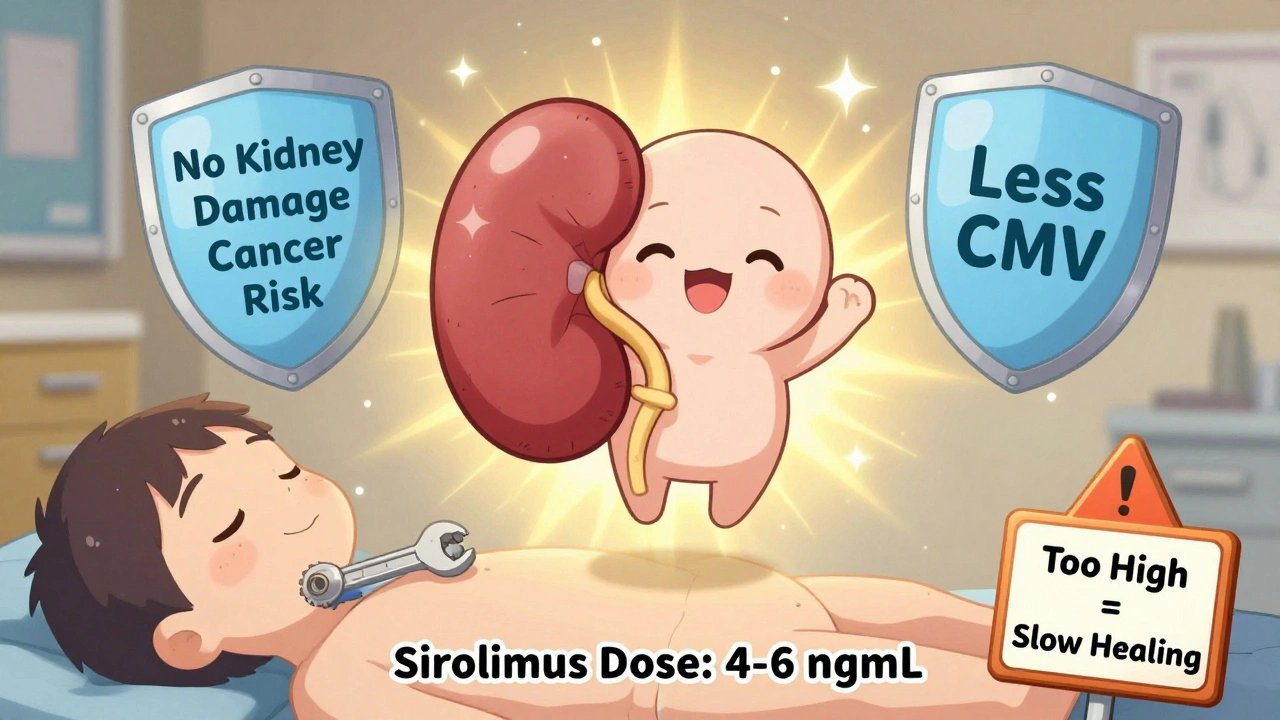
Why Use Sirolimus at All?
If it slows healing, why not just avoid it? Because it has unique benefits no other immunosuppressant offers:- No kidney damage: Unlike tacrolimus or cyclosporine, sirolimus doesn’t harm the transplanted kidney over time. That’s huge for long-term graft survival.
- Lower cancer risk: Transplant patients have a 2-4 times higher risk of skin and other cancers. Sirolimus has anti-cancer properties-it can slow tumor growth. In patients with a history of skin cancer or Kaposi’s sarcoma, it’s often the preferred choice.
- Less viral infections: Studies show lower rates of CMV and EBV infections compared to calcineurin inhibitors.
What Can Be Done to Reduce Risk?
If a patient needs sirolimus, here’s what works:- Optimize nutrition: Start protein supplements (1.2-1.5 g/kg/day) and check albumin levels pre-op.
- Quit smoking: At least 4 weeks before surgery. Even nicotine patches are risky.
- Control blood sugar: HbA1c below 7% is ideal. Use insulin if needed.
- Use wound care best practices: Keep incisions clean, avoid tension, use negative pressure dressings if needed.
- Monitor healing closely: Check for redness, swelling, fluid buildup, or delayed closure. Don’t wait for infection to set in.
- Consider alternatives: If healing is a major concern, use belatacept (a non-nephrotoxic alternative) or a calcineurin inhibitor with lower doses.
The Bottom Line
Sirolimus isn’t the enemy of wound healing-it’s a tool that needs careful handling. The old rule of avoiding it entirely after surgery is outdated. Today’s approach is smarter: assess risk, delay if needed, dose low, monitor closely, and optimize the patient first. Patients who are healthy, well-nourished, and non-smokers can often start sirolimus safely within 7-10 days. Those with multiple risk factors need more time. The goal isn’t to avoid sirolimus-it’s to use it where it does the most good and the least harm. The data is clear: with the right patient selection and timing, sirolimus can be used safely in transplant recipients without sacrificing long-term outcomes. The real mistake isn’t using it-it’s using it the same way for everyone.Can sirolimus cause wound infections?
Yes, sirolimus can increase the risk of wound infections by slowing down the immune response and tissue repair. However, infection rates are often tied to other factors like obesity, diabetes, or smoking. In one study, 19.2% of patients on sirolimus developed infections after dermatologic surgery, compared to 5.4% in controls-but the difference wasn’t statistically significant. The real risk comes from combining sirolimus with other immunosuppressants or poor pre-op health.
How long should I wait after surgery to start sirolimus?
Most transplant centers wait 7 to 14 days after major surgery before starting sirolimus. For high-risk patients (obese, diabetic, smoker), wait closer to 10-14 days. For low-risk patients with clean, small incisions, some centers start as early as day 5-7. The key is to wait until the incision shows signs of stable healing-no drainage, no redness, no separation.
Is sirolimus safe after skin surgery?
Yes, studies show sirolimus is generally safe after minor skin procedures like excisions or biopsies. The Mayo Clinic found no significant increase in complications in transplant patients on sirolimus who had dermatologic surgeries. This is likely because these wounds are small, superficial, and heal quickly. The risk is much higher after abdominal or chest surgeries where tissue tension and fluid buildup are common.
What’s the ideal sirolimus level after transplant?
During the first 30 days after transplant, aim for trough levels between 4-6 ng/mL. Higher levels (above 8 ng/mL) significantly increase the risk of poor wound healing. After 30 days, levels can be raised to 8-12 ng/mL for better rejection prevention. Regular blood tests are critical in the early phase to adjust doses based on healing, not just rejection markers.
Can I switch from tacrolimus to sirolimus if I have kidney damage?
Yes, switching from tacrolimus or cyclosporine to sirolimus is a common strategy for patients developing kidney damage from calcineurin inhibitors. Sirolimus doesn’t harm the kidneys and can even help stabilize long-term function. However, if the patient has recent surgery or poor wound healing, the switch should be delayed until the wound is fully closed-usually 4-6 weeks post-op. Monitor healing closely after the switch.

11 Comments
Linda Migdal
Sirolimus is a classic example of how pharmaceutical companies weaponize molecular biology to create dependency. Blocking mTOR sounds elegant until you realize you're sabotaging tissue regeneration. The FDA should've flagged this sooner. We're trading short-term graft survival for long-term morbidity-and hospitals are fine with it because they get paid for complications. This isn't medicine. It's profit-driven trauma engineering.
Shannon Gabrielle
So let me get this straight-we’re delaying a life-saving drug because fat people and smokers can’t heal? Wow. Just wow. Next they’ll ban insulin because diabetics have slow wounds. Let’s just give everyone a wheelchair and call it a day. The real problem isn’t sirolimus-it’s the fact we treat patients like broken machines instead of humans with systemic issues.
Nnaemeka Kingsley
Man, this post really opened my eyes. I didn't know sirolimus could mess up healing like that. My cousin got a transplant and they started him on it right away-he got infected bad. Maybe they should check your BMI and sugar before giving the drug. Simple stuff, really.
Kshitij Shah
Classic Western medical arrogance. You blame the patient’s body for the drug’s side effects. In India, we use turmeric, neem, and honey on wounds-no mTOR blockers needed. But hey, why bother with ancient wisdom when you’ve got a $2000 pill that ‘works’? #PharmaOverEverything
Sean McCarthy
Wait. Wait. Wait. You’re telling me that a drug that suppresses mTOR-yes, mTOR-is also suppressing VEGF, fibroblasts, collagen, and angiogenesis? That’s not a side effect. That’s the primary mechanism. And you’re surprised it delays healing? This isn’t a dilemma. It’s basic pharmacology. The real question is: why did it take 15 years for hospitals to catch on?
Tommy Walton
Sirolimus: the Nietzschean drug. It doesn't just suppress immunity-it forces the body to transcend its biological limits. The wound doesn't heal? Good. That means the body is evolving beyond frailty. 🌱⚡️
James Steele
The data is unequivocal: sirolimus is not a liability-it’s a biomarker of systemic resilience. The fact that clinicians still treat it as a binary risk factor reveals a profound epistemological deficit in modern transplant medicine. We are managing outcomes, not optimizing biological potential. The 4-6 ng/mL paradigm is a relic of reductionist thinking. We need systems biology. We need predictive modeling. We need to stop treating patients like widgets on an assembly line.
Louise Girvan
Who funds these studies? Who controls the guidelines? Who decides what's 'low-risk'? I've seen patients die because they were 'low-risk' and got sirolimus on day 5. The FDA is in bed with AstraZeneca. The 'no significant difference' studies? Published by the same labs that make the drug. Wake up. This isn't science-it's a cover-up.
soorya Raju
They say sirolimus helps with cancer? Lmao. What if it's just making tumors grow slower so they don't get caught until they're stage 4? That's not a benefit-that's a trap. And what about lymphoceles? Those aren't 'complications'-they're the body screaming for help. They just ignore it and call it 'expected'. I'm not buying it.
Dennis Jesuyon Balogun
Let me say this plainly: sirolimus isn't the villain. The villain is the system that treats patients as data points instead of people. A diabetic smoker with a BMI of 35? They’re not 'high-risk'-they’re a symptom of a broken food system, a broken healthcare access model, and a broken social safety net. We don’t need to delay sirolimus-we need to fix the conditions that made them high-risk in the first place. Healing isn’t just about tissue. It’s about justice.
Grant Hurley
My uncle got his kidney transplant last year. They waited 12 days to start sirolimus. He’s been fine since. No infections, no leaks, just chill vibes. The key? He quit smoking, ate protein like it was his job, and walked 2 miles every day. No magic pill. Just basic human care. Sometimes the best treatment is just… listening.