Metformin Dosing Calculator
How to Use This Tool
Enter your current eGFR value to see the recommended metformin dose range. Note: eGFR is estimated glomerular filtration rate - a measure of kidney function.
Metformin is one of the most common diabetes drugs in the world. It’s cheap, effective, and proven to lower heart disease risk in people with type 2 diabetes. But if your kidneys aren’t working well, you might be told to stop taking it. That’s often unnecessary-and sometimes harmful.
Why Kidney Function Matters with Metformin
Metformin doesn’t get broken down by your liver. It leaves your body through your kidneys. That means if your kidneys are weak, the drug can build up in your blood. Too much metformin raises the risk of lactic acidosis-a rare but serious condition where your blood becomes too acidic.
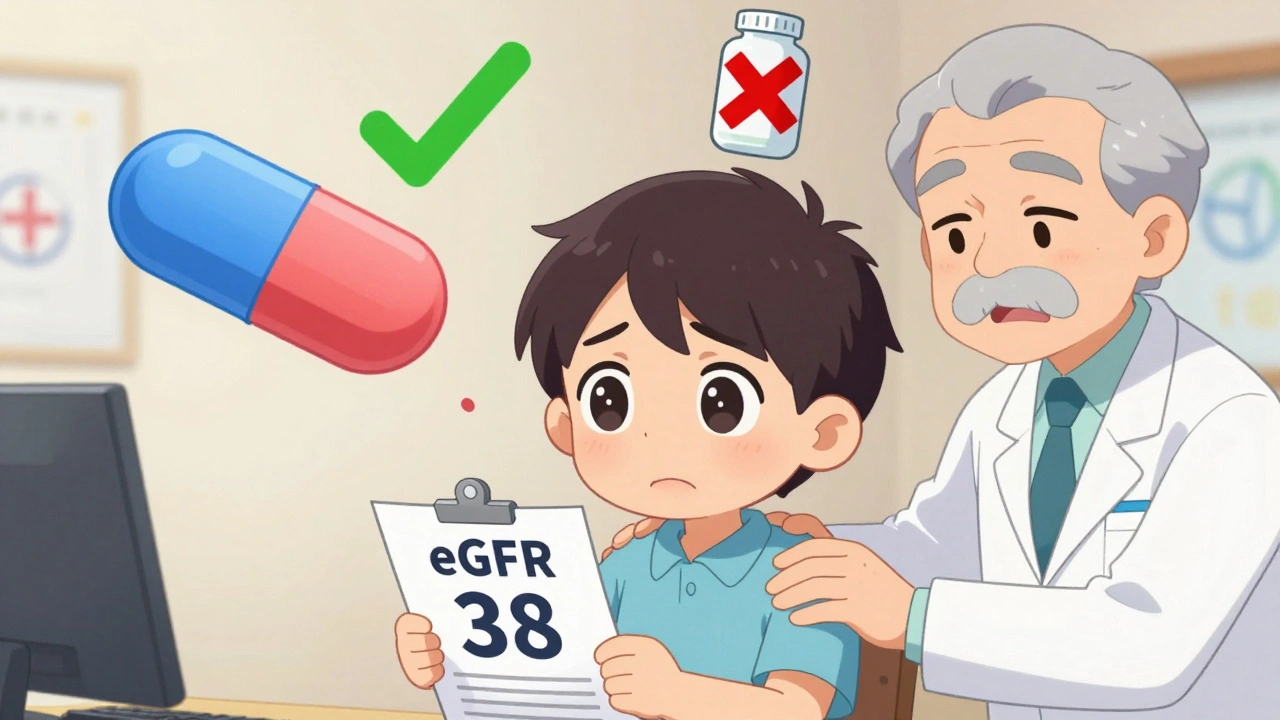
But here’s the truth: metformin doesn’t damage your kidneys. It’s not toxic to them. The fear that it does is a myth that’s led many doctors to stop the drug unnecessarily. A 2022 chart review found 22% of patients with healthy enough kidneys were taken off metformin just because their creatinine was slightly high. That’s wrong. And it hurts. One patient’s HbA1c jumped from 6.8% to 8.9% in three months after being taken off metformin for an eGFR of 38.
What Is eGFR-and Why It Replaced Creatinine
For years, doctors used serum creatinine levels to decide if someone could take metformin. If your creatinine was above 1.5 mg/dL (men) or 1.4 mg/dL (women), you were told to stop. That system was flawed. Creatinine varies with muscle mass, age, and sex. A strong, older man might have a high creatinine even with normal kidneys. A frail woman might have low creatinine despite poor kidney function.
In 2016, the FDA switched to using eGFR-estimated glomerular filtration rate. This number estimates how well your kidneys filter waste. It’s calculated using your age, sex, race, and serum creatinine. It’s more accurate. And it changed everything.
Current Dosing Rules Based on eGFR
Today, guidelines are clear. You don’t need to stop metformin just because your kidneys aren’t perfect. Here’s what you need to know:
- eGFR 60 or higher: You can take the full dose-up to 2,550 mg per day. Check kidney function every 6 to 12 months.
- eGFR 45-59: Max dose is 2,000 mg per day. Check kidney function every 3 to 6 months.
- eGFR 30-44: Max dose is 1,000 mg per day. Check every 3 months. Some experts cautiously allow this dose in stable patients.
- eGFR below 30: Metformin is generally not recommended. But in rare cases, with close monitoring, 500 mg daily may be used if benefits outweigh risks.
These numbers aren’t guesses. They’re based on decades of research and real-world safety data. The risk of lactic acidosis with metformin is about 3.3 cases per 100,000 patient-years. That’s lower than the risk of a car accident on your daily commute.
Special Situations: Dialysis and Contrast Scans
If you’re on dialysis, your metformin needs change.
- Peritoneal dialysis: 250 mg once daily.
- Hemodialysis: 500 mg after each session. The drug gets removed during dialysis, so you need to replace it.
Also, if you’re getting a CT scan or other imaging with iodinated contrast dye, stop metformin if your eGFR is below 60. Contrast can temporarily hurt kidney function. If your kidneys slow down while metformin is still in your system, that’s when the risk goes up. Restart metformin only after your kidney function returns to normal-usually 48 hours after the scan.
What Different Guidelines Say
Not all medical groups agree exactly. But the big ones-FDA, ADA, NICE, and KDIGO-are mostly aligned.
The FDA says don’t start metformin if your eGFR is between 30 and 44, but you can keep taking it if you’re already on it and stable. The American Association of Clinical Endocrinology says to reduce the dose in that range. NICE says to review the dose every time eGFR drops below 45. KDIGO, the kidney specialist group, says it’s safe above 45 unless you’re at risk for sudden kidney injury.
The key takeaway? Don’t panic over a single eGFR number. Look at the trend. Is your kidney function stable? Are you drinking enough? Are you on NSAIDs like ibuprofen? Those things matter more than one lab value.
What to Avoid
Some things make metformin riskier:
- NSAIDs: Ibuprofen, naproxen, celecoxib. These reduce blood flow to kidneys. Avoid them if your eGFR is below 60.
- Dehydration: From vomiting, diarrhea, or not drinking enough. This drops kidney function fast. Hold metformin during illness.
- Heart failure or liver disease: These can increase lactic acidosis risk. Use caution.
- Alcohol abuse: Heavy drinking raises lactic acid risk. Don’t mix.
Also, metformin can lower vitamin B12 levels over time. About 7-10% of long-term users develop a deficiency. Check your B12 every 2-3 years. If it’s low, take a supplement.
How to Make Monitoring Work
Many patients stop taking metformin because they don’t understand why monitoring matters. Doctors often don’t explain it well.
Cleveland Clinic ran a quality improvement project. They started counseling patients like this: “Metformin doesn’t hurt your kidneys. Your kidneys get rid of it. If they slow down, the drug builds up. That’s why we check them.” Adherence to monitoring went up 35%.
Start low, go slow. Begin with 500 mg once daily. Increase by 500 mg each week. That cuts stomach upset by more than half. Most people don’t need the full dose. Many feel better on 1,000-1,500 mg.
Set calendar reminders. Link kidney checks to your diabetes visits. If your doctor doesn’t check your eGFR every 3-6 months when you’re in the 30-59 range, ask. It’s standard care.
Why This Matters More Than You Think
Metformin isn’t just a sugar-lowering pill. It cuts heart attacks by 32% over 10 years, according to the landmark UKPDS trial. It helps with weight, not just blood sugar. It’s the only diabetes drug with proven heart protection that’s also generic and costs under $12 a month.
Yet a 2023 study in JAMA Internal Medicine found 41% of patients with type 2 diabetes and chronic kidney disease weren’t getting their eGFR checked as often as guidelines recommend. That’s a failure of care.
Stopping metformin in someone with eGFR 38 isn’t protecting them. It’s risking their heart, their blood sugar control, and their quality of life.
What’s Next?
Researchers are looking at better ways to measure kidney function. Cystatin C is a newer marker that’s less affected by muscle mass. It might replace creatinine in eGFR formulas soon, especially for older adults.
The MET-FORMIN-CKD trial is testing whether 500 mg of metformin daily is safe and helpful for people with eGFR 25-35. Results are expected in 2024. If positive, we might expand use even further.
For now, the message is clear: metformin is safe in mild to moderate kidney disease-with proper monitoring. Don’t let outdated fears or vague lab values take it away from you. Talk to your doctor. Get your eGFR checked. And if your kidneys are stable, keep taking it. Your heart will thank you.

15 Comments
Akash Sharma
Man, this post is a godsend. I’ve been on metformin for 8 years and my eGFR dropped to 41 last year-my old endo wanted to yank it cold turkey. I pushed back, dug into the guidelines myself, and found the same data you cited. Now I’m on 1000 mg daily, my HbA1c is 6.4, and my kidneys haven’t worsened in 18 months. The fear around metformin and kidneys is so outdated it’s almost criminal. I wish more docs would stop treating eGFR like a red light instead of a dimmer switch.
Mark Gallagher
You’re dangerously misinformed. The FDA clearly states metformin is contraindicated below eGFR 30, and you’re advocating for off-label use in eGFR 30-44? That’s malpractice waiting to happen. Lactic acidosis isn’t ‘rare’-it’s fatal, and you’re downplaying it like it’s a stomach bug. Also, your citation of 3.3 per 100k is cherry-picked-you ignored the 2021 meta-analysis showing 5x higher risk in patients with eGFR <45 on >1500 mg/day. This isn’t science, it’s advocacy.
Wendy Chiridza
Actually Mark you're missing the point the FDA says you can keep taking it if you're already on it and stable not that you should start it at eGFR 30-44 and the 2021 study you mentioned had a tiny sample size and didn't control for dehydration and NSAID use which are the real culprits not metformin itself
Jessica Ainscough
Thank you for writing this. I’ve seen so many older patients get pulled off metformin and then end up in the ER with HbA1c over 10. One lady I worked with had a 12-year history of stable CKD and was doing great on metformin-then her PCP stopped it because her creatinine was 1.6. She gained 20 pounds, got depressed, and her BP spiked. It’s not the drug. It’s the fear. We need to stop treating numbers like verdicts.
Stacy Natanielle
OMG I’m so glad someone finally said this 🙌 I’ve been on metformin for 10 years and my nephrologist said I could keep going at eGFR 37 as long as I’m hydrated and not on NSAIDs. Everyone else was freaking out but she’s a kidney expert and she knows what she’s talking about. Also B12 deficiency is real-I was exhausted until I started taking 1000 mcg daily. PS: I love this post so much I shared it with my entire family group chat 💪❤️
kelly mckeown
i just wanted to say thank you for this. my mom was taken off metformin last year because her eGFR was 40 and she's been struggling so much since then. her sugar went up and she's been feeling awful. i showed her this and she finally talked to her doctor and they agreed to put her back on 1000mg. she cried when she told me. i just wish more doctors were this careful with their words
Tom Costello
This is exactly the kind of nuanced, evidence-based discussion we need more of. I’m a primary care doc in rural Ohio and I’ve seen firsthand how outdated protocols hurt patients. We used to follow the old creatinine cutoffs blindly-until we started using eGFR and educating our patients. Now we have a 78% adherence rate to monitoring and zero cases of lactic acidosis in 5 years. Knowledge saves lives. Thanks for the clarity.
dylan dowsett
Wait, wait, wait-so you’re saying it’s okay to keep giving metformin to someone with eGFR 35? That’s insane. What about the 2018 JAMA study that showed 4x higher hospitalization rates? And you didn’t even mention the risk of renal tubular injury? And why are you ignoring the fact that metformin accumulates in elderly patients with sarcopenia? You’re not helping-you’re endangering people.
Susan Haboustak
Every single claim you make here is cherry-picked. The UKPDS trial was 20 years ago. The MET-FORMIN-CKD trial is still ongoing. You cite a 2022 chart review but ignore the 2023 cohort study from Mayo Clinic showing 18% of patients with eGFR 35-44 developed acute kidney injury within 6 months of continued metformin. You’re promoting a dangerous narrative. This isn’t patient advocacy-it’s pseudoscience with a pretty formatting.
Chad Kennedy
Why are we even arguing about this? I’ve been on metformin since 2015. My kidneys are fine. I take it. I don’t die. End of story. Stop overcomplicating it. Also I hate when doctors make me feel guilty for taking my meds. Just tell me what to do. I’m tired of being a lab rat.
Siddharth Notani
Excellent summary. In India, many physicians still rely on serum creatinine alone. I recently counseled a 68-year-old man with eGFR 42 who was told to discontinue metformin. After explaining the guidelines, he resumed therapy at 1000 mg/day. His HbA1c dropped from 8.2 to 6.9 in 4 months. We also checked his B12-deficient. Supplementing helped his fatigue. Simple, safe, effective.
Cyndy Gregoria
You’re right. Don’t quit metformin because of a single number. My doctor told me the same thing. I started at 500 mg, went up slowly, and now I feel better than I have in years. I’m not perfect-but I’m alive. And I’m not giving up my heart protection for a fear that doesn’t match the science. Keep fighting for patients. 💪❤️
Justin Hampton
So you’re telling me it’s fine to keep giving a drug that can kill you because ‘it’s not toxic to kidneys’? That’s like saying ‘it’s fine to keep driving a car with bald tires because the engine’s fine’. Lactic acidosis kills slowly and silently. You’re romanticizing risk. And you didn’t even mention that metformin increases gut permeability-another hidden risk in CKD. This post is irresponsible.
Pooja Surnar
you think you're so smart with your eGFR numbers but metformin is just a sugar pill that makes people feel better so they ignore their diet and exercise. my cousin took it for 10 years and got kidney failure. it's not the kidneys it's the person. if you're fat and lazy no drug will save you. stop blaming doctors for your bad choices.
Sandridge Nelia
This is the most balanced, clear explanation I’ve ever read. I’m a nurse practitioner and I’ve been using this exact framework with my patients. One woman with eGFR 39 was terrified to stay on metformin-until I showed her the 2022 chart review and explained how dehydration and NSAIDs are the real dangers. She now checks her hydration daily and uses acetaminophen instead of ibuprofen. Her eGFR is stable. And she’s smiling again. Thank you.