After a heart attack, life doesn’t go back to how it was before. But it doesn’t have to stop, either. Recovery isn’t about getting back to normal-it’s about building a new normal. One that’s safer, stronger, and more sustainable. The key? Three things: the right medications, the right food, and the right amount of movement. Not all at once. Not all perfectly. But consistently, over time.
Medications: Your Lifeline, Not a Burden
You’ll leave the hospital with a handful of new pills. Maybe more than you’ve ever taken before. It’s overwhelming. But each one has a job. Skipping doses or stopping because you “feel fine” is one of the biggest mistakes people make. Your heart was damaged. These drugs are there to stop more damage from happening.
Common medications after a heart attack include beta-blockers to slow your heart rate and lower blood pressure, ACE inhibitors or ARBs to reduce strain on your heart, statins to lower cholesterol and stabilize plaque in your arteries, and aspirin or another antiplatelet drug to prevent clots. Some may also need aldosterone antagonists or nitrates depending on their condition.
The NHS recommends carrying a written list of all your medications-name, dose, and why you take it. Keep it in your wallet or phone. Pharmacists are part of your recovery team. They can explain what each pill does, warn you about interactions, and help you set up pill boxes or reminders. If you’re confused, ask. There’s no such thing as a silly question when your heart’s on the line.
Diet: What You Eat Is Your Next Medicine
Forget fad diets. After a heart attack, your plate becomes your toolkit. The goal isn’t weight loss alone-it’s reducing inflammation, lowering blood pressure, and keeping your arteries clear.
Start here: cut out processed foods. That means less salt, less added sugar, and fewer packaged snacks. Swap white bread for whole grains. Choose lean proteins like fish (especially salmon, mackerel, or sardines), beans, lentils, and skinless chicken. Load up on vegetables-colorful ones. Broccoli, spinach, carrots, peppers. They’re full of fiber and antioxidants that help your heart heal.
Fats matter. Not all fats are bad. Avoid trans fats (look for “partially hydrogenated oils” on labels) and limit saturated fats from butter, fatty meats, and full-fat dairy. Instead, get your fats from olive oil, avocados, nuts, and seeds. A handful of almonds or walnuts a day can make a real difference.
Cardiac rehab programs often include a registered dietitian who builds a plan around your tastes, culture, and health needs. Maybe you love rice and beans? That’s fine. Just make sure it’s not drowned in salt or oil. Maybe you’re used to sugary tea? Try switching to herbal tea or water with lemon. Small changes add up.
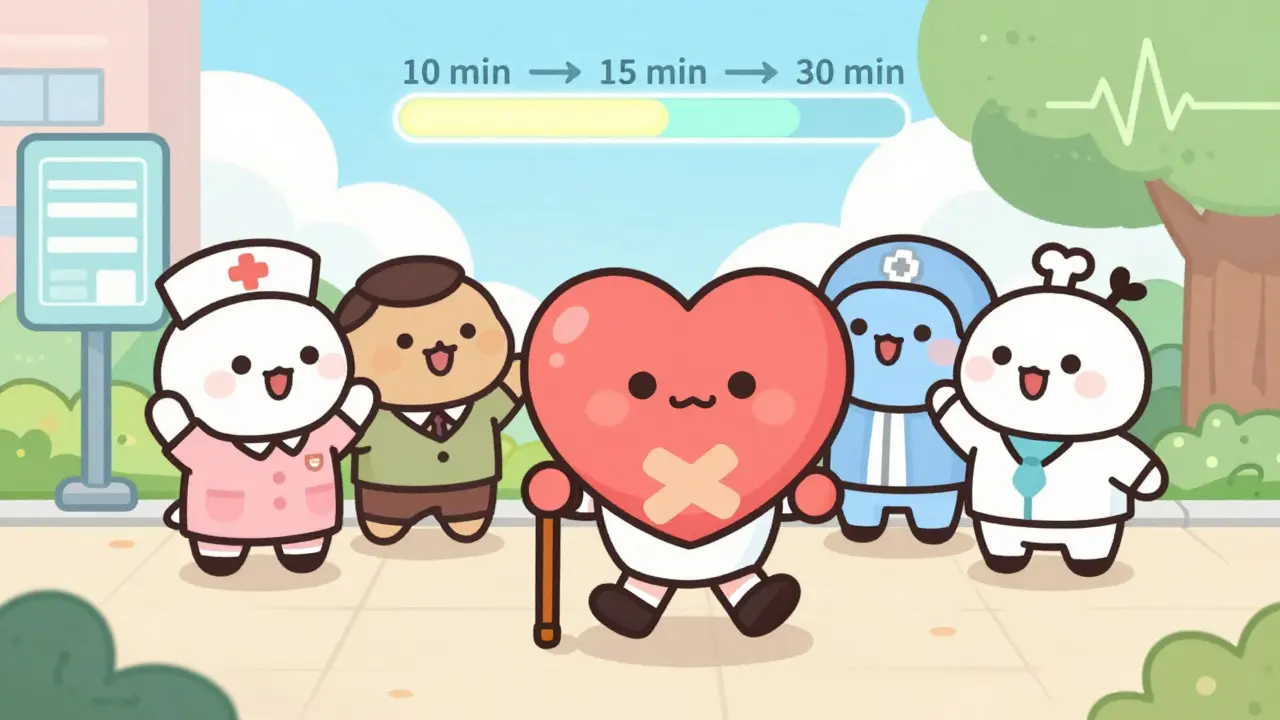
Activity: Move, But Don’t Rush
The first week after going home, you’ll feel tired. Weak. Like you’ve run a marathon just by walking to the kitchen. That’s normal. Your heart muscle was injured. It needs rest to heal.
But rest doesn’t mean lying still. The NHS advises starting with light activity: walking up and down stairs a few times a day, or a short walk around the block. Gradually increase. Add a minute here, a minute there. Aim for 10 minutes a day at first. Then 15. Then 20. Within weeks, you should be working toward 30 minutes most days.
Aerobic exercise is the gold standard. Walking, cycling on a stationary bike, swimming-these are all safe and effective. They strengthen your heart, improve circulation, and help lower blood pressure. Avoid heavy lifting or sudden bursts of effort in the early weeks. Your rehab team will guide you.
Cardiac rehabilitation is not optional. It’s the backbone of recovery. These programs run for 8 to 12 weeks and include supervised exercise, education on your condition, stress management, and emotional support. You’ll be with others who’ve been through the same thing. You’ll learn how to listen to your body. When to push. When to stop. Many people say rehab gave them their life back.
Recovery Isn’t Linear
Some days you’ll feel great. Others, you’ll drag yourself through the motions. That’s okay. Recovery isn’t a straight line. It’s a spiral. You’ll circle back to the same feelings-fear, frustration, fatigue-multiple times.
One study from the American Heart Association found that people who stuck with cardiac rehab for at least 12 weeks had a 25% lower risk of having another heart attack or dying from heart disease. That’s not a small number. It’s life-changing.
Don’t compare yourself to others. Someone else might be jogging by week six. You might still be walking. That’s fine. Your heart is yours alone. Progress is measured in consistency, not speed.
Don’t Ignore the Mind
It’s easy to focus on the body. But the emotional toll is real. Anxiety. Depression. Fear of another attack. These aren’t signs of weakness. They’re normal responses to a life-threatening event.
The NHS includes psychological support as part of every cardiac rehab program. Talking to a counselor, joining a peer group, or even just opening up to your partner can help. If you’re feeling down for more than two weeks, ask your doctor. There are safe, effective treatments for depression after a heart attack-and they improve physical recovery too.
Follow-Up: Keep Showing Up
You’ll have a check-up four to six weeks after leaving the hospital. That’s not just a formality. It’s your chance to ask questions, report symptoms, and adjust your plan. Don’t wait until you’re in crisis to call your doctor. Call if you notice new chest discomfort, unusual shortness of breath, swelling in your legs, or sudden weight gain. These could be signs your heart is struggling.
Long-term, you’ll need regular blood tests to monitor cholesterol, kidney function, and electrolytes. Blood pressure checks. ECGs. Your care team will set a schedule. Stick to it.
What Comes Next?
After three months, many people feel like themselves again. But recovery doesn’t end there. It evolves. You’ll keep taking your meds. You’ll keep eating well. You’ll keep moving. These aren’t temporary fixes. They’re lifelong habits.
Some people go back to work. Others retire early. Some take up gardening. Others join a walking group. There’s no one right path. But there is one rule: never stop caring for your heart.
Every choice you make-from the food on your plate to the walk you take after dinner-is a step toward a longer, stronger life. You’ve already survived the worst. Now, build the rest.
How long does it take to recover from a heart attack?
Recovery varies by person. Most people start feeling better in 2 to 6 weeks, but full recovery can take up to 3 months. The NHS and Cleveland Clinic both stress that rushing recovery increases the risk of complications. Listen to your body and follow your rehab plan.
Can I drive after a heart attack?
In the UK, you must not drive for at least 4 weeks after a heart attack. If you have a Group 1 license (car or motorcycle), you can resume driving after 1 week if you had a simple heart attack with no complications and no symptoms. For Group 2 (lorries, buses), you must wait 3 months and get clearance from your doctor. Always check with your GP or DVLA for your specific case.
Do I need to take heart medications forever?
For most people, yes. Medications like statins, aspirin, and beta-blockers aren’t just for the first few months-they’re meant to protect your heart for life. Stopping them without medical advice can lead to another heart attack. If side effects are a problem, talk to your doctor. There are often alternatives.
Is it safe to have sex after a heart attack?
Yes, for most people. Sexual activity is similar in effort to climbing two flights of stairs. If you can walk briskly or do light housework without chest pain or dizziness, you’re likely ready. Talk to your doctor if you’re unsure. Emotional anxiety is common-this is normal, and support is available.
What if I can’t afford my medications?
In the UK, you’re entitled to free prescriptions if you’ve had a heart attack. Ask your GP for an exemption certificate (MedEx). If you’re outside the UK, many pharmaceutical companies offer patient assistance programs. Your pharmacist or cardiac rehab team can help you find options. Never skip doses because of cost-there are always solutions.